*Editor’s Note: Article contributed by Adele Allison, director of Provider Innovation Strategies, DST Health Solutions. Ms. Allison will be a presenter during the Medical Association’s 2017 Annual Meeting and Business Session on April 14-15 in Montgomery.
The Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) accelerates the pace of change in the movement toward value-based payment (VBP).1 With an effective date of Jan. 1, 2019, MACRA requires Medicare providers to choose from two defined reimbursement paths that link quality to payment: the Merit-Based Incentive Payment System (MIPS) or advanced Alternative Payment Models (APMs).2 After considering more than 4,000 comments to the proposed rule considered, CMS released the final rule on Oct. 14,3 officially rolling out the Quality Payment Program (QPP).
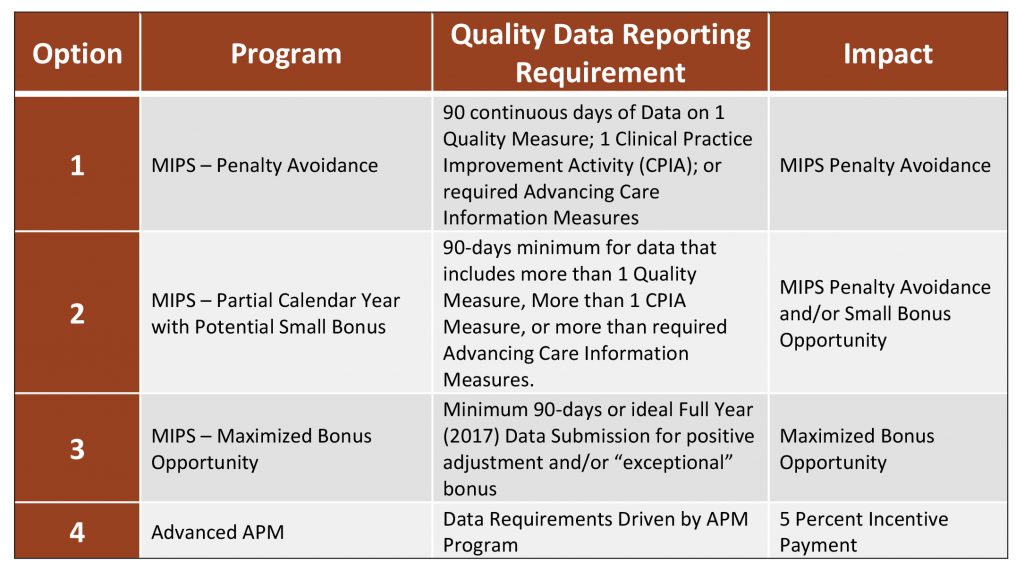
CMS has outlined phases for MIPS and APMs to go into effect over a timeline through 2021 and beyond. The first CMS-proposed performance reporting period begins Jan. 1, 2017 (for payment adjustments starting in 2019). Under MACRA, Medicare revenue may be adjusted upward or downward by as much as 4 percent in 2019 (based on performance in 2017) and up to 9 percent in later years.4 To respond to the rapid program launch, CMS announced in the final rule a “Pick-Your-Pace” option for 2017, allowing a range of provider quality reporting choices to comply with MACRA.5 Nevertheless, MACRA heralds a new era in provider payment where effectiveness, efficiency and performance data will determine each clinician’s economic viability. This article will explore the essential strategies providers should consider to evolve their culture and technologies towards these new value-based payments.
Impact of MACRA: The Timing
MACRA is a Medicare cost containment law grounded in quality performance. It seeks to move health care systems and providers to advance alternative payment arrangements over time, but as quickly as the industry will allow. In the mature stages, physician practices will be expected to understand and manage the risk of care associated with attributed patient populations. While population-based payment, the most advanced phase, is the desired destination, few of today’s providers are expected to be ready to assume this level of risk. Since most providers aren’t ready to take on risk, CMS expects MIPS to be the path initially most traveled by providers – predicting 761,342 clinicians to be precise.6 Yet, even MIPS is being recognized by CMS as a lofty goal in 2017.
Milestones Toward Increasing Levels of Risk-Bearing
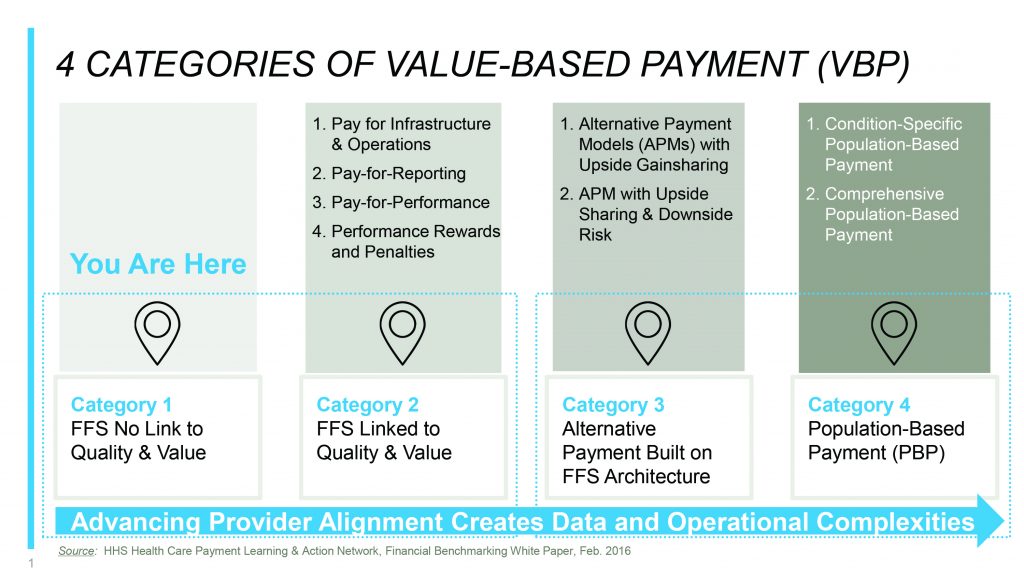
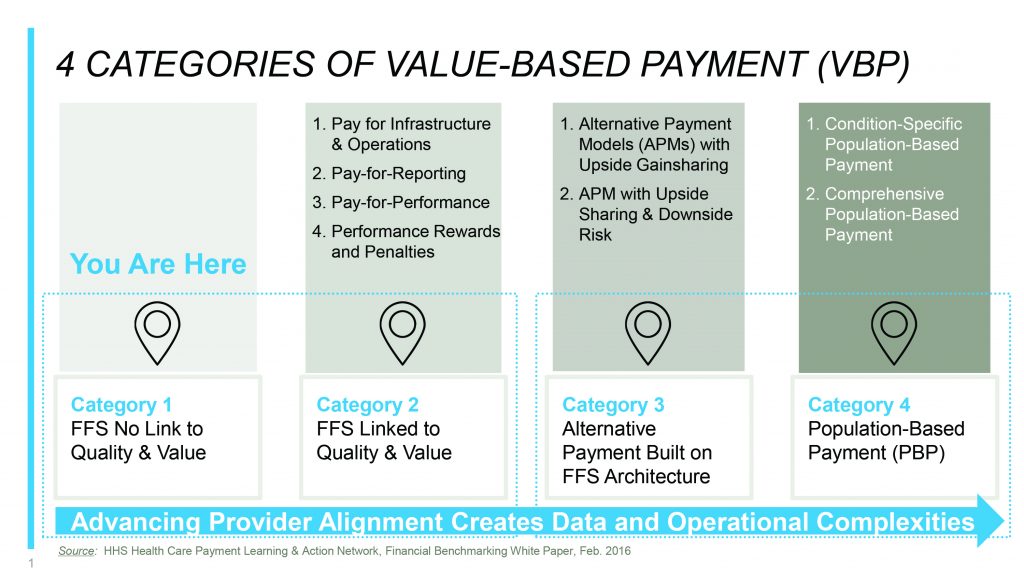
The path forward to align value-based payment models across private and public health plans and health systems has been laid out by the recently formed Health Care Payment Learning and Action Network (HCPLAN). The HCPLAN is a public-private collaboration of health plans, providers, patients, employers, consumers, states, federal agencies and other partners seeking to accelerate the adoption of alternative payment models that reward quality and value in health care.
Among other things, the HCPLAN has defined a framework of four categories as milestones along a payment continuum. Each category moves toward increasing levels of risk-bearing, value-based care, and payment innovation (see Figure 1).7 Physicians and other clinicians can use this framework to evaluate the status of their current payer agreements in this journey. They can also use this framework to begin developing plans to evolve further along this continuum.
Four Categories of Value-Based Payment
Category 1 Traditional fee-for-service (FFS) with no link to quality or value. Category 1 represents traditional payment models typically built on fee schedules and diagnostic related groups (DRGs).
Category 2 FFS linked to measures of quality and value. Providers are paid differentially based on measures of quality, yet providers continue to receive a fee for each service. MIPS is a Category 2 payment arrangement as is the Blue Cross and Blue Shield of Alabama Quality Management Program.8
Category 3 Alternative payment built on an FFS infrastructure. Providers begin taking limited risk with alternative payment models that span across the continuum of care. A retrospective bundled payment fits in this category, as does shared savings under an Accountable Care Organization (ACO). Category 3 arrangements that include “significant but not excessive” risk-bearing qualify as advanced APMs under MACRA. Qualified participants in CMS advanced APMs will not be subject to MIPS and will be eligible to receive a 5 percent incentive payment. Available in 14 regions, CMS has elevated the expanded medical home, a risk-sharing PCMH known as the Comprehensive Primary Care Plus (CPC+), as an example of a qualifying advanced APM under MACRA.9
Category 4 This is a population-based payment. Under Category 4, payment is not triggered by clinical service delivery, but rather the payer makes a population-based payment to the provider to assume responsibility over a defined period of time. Category 4 clinicians embrace advanced risk-bearing models often across the care continuum; shared risk for an attributed patient population that may be condition-specific or global. Like more than nominal risk arrangements under Category 3, CMS will recognize Category 4 providers as QPs under advanced APMs and not subject to MIPS.
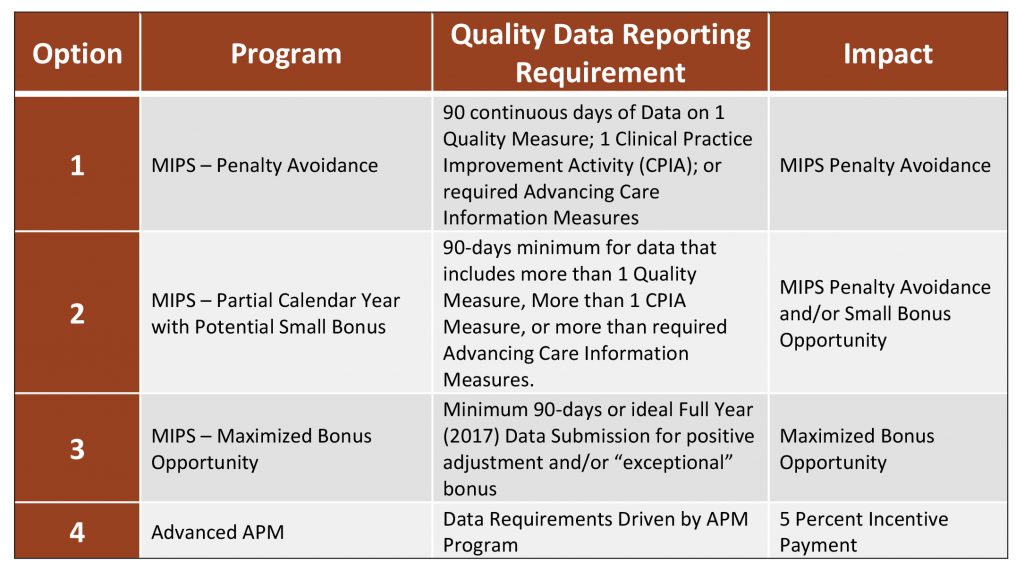
CMS Outline of a “Pick-Your-Pace” Plan
Since the first MIPS performance period is set for Calendar Year 2017 and the final rule governing the details of MACRA was not released until Oct. 14, 2016, providers will have very little time to plan, prepare and implement necessary changes to succeed. In response to industry concerns and comments, CMS will allow MACRA providers to “Pick Your Pace” in 2017 under the following structure in Figure 2.10
Leveraging Data for Population Health Management
Through MACRA, CMS is leading change in payment reform that will permeate to other segments of health care. Providers need to think strategically about alignment with emerging quality measures and payment structures. Today is an opportune time for providers to begin collaborating more fully with each other and health plans to achieve higher levels of measurable care and payment; and, measurement is driven by data. Providers must begin thinking about assuming collective responsibility for attributed patient populations across the health delivery system as this is where payment is heading.
To do this, practitioners should leverage combined data for population health management as a provider community. The Meaningful Use programs provided physicians and other clinicians with growing visibility into their individual patient populations. Where the payer-provider relationship is one-on-one, such as under traditional fee-for-service (FFS) contracts, individual provider technical capabilities may be sufficient to meet preliminary demands for managing patient populations. Under a growing plethora of PBP models, many different types of clinicians (primary care physicians, specialists, physician assistants, nurse practitioners, nurse specialists, dentists, physical therapists, and others) may be paid as part of a collective for a shared patient. This will be driven by composite measurements that require a view of data beyond the four walls of the individual provider enterprise.
Payers have had this aggregated data view for decades through the most foundational data-source in the U.S. – claims data. Your claims process is not just a means of getting paid. Claims are a reporting vehicle where the nuances of your patient population are communicated and assessed by a payer. More and more, payers are beginning to share this aggregated population data with providers to assist with resource management, assessment of disease burden and outcomes measurement across the care continuum.
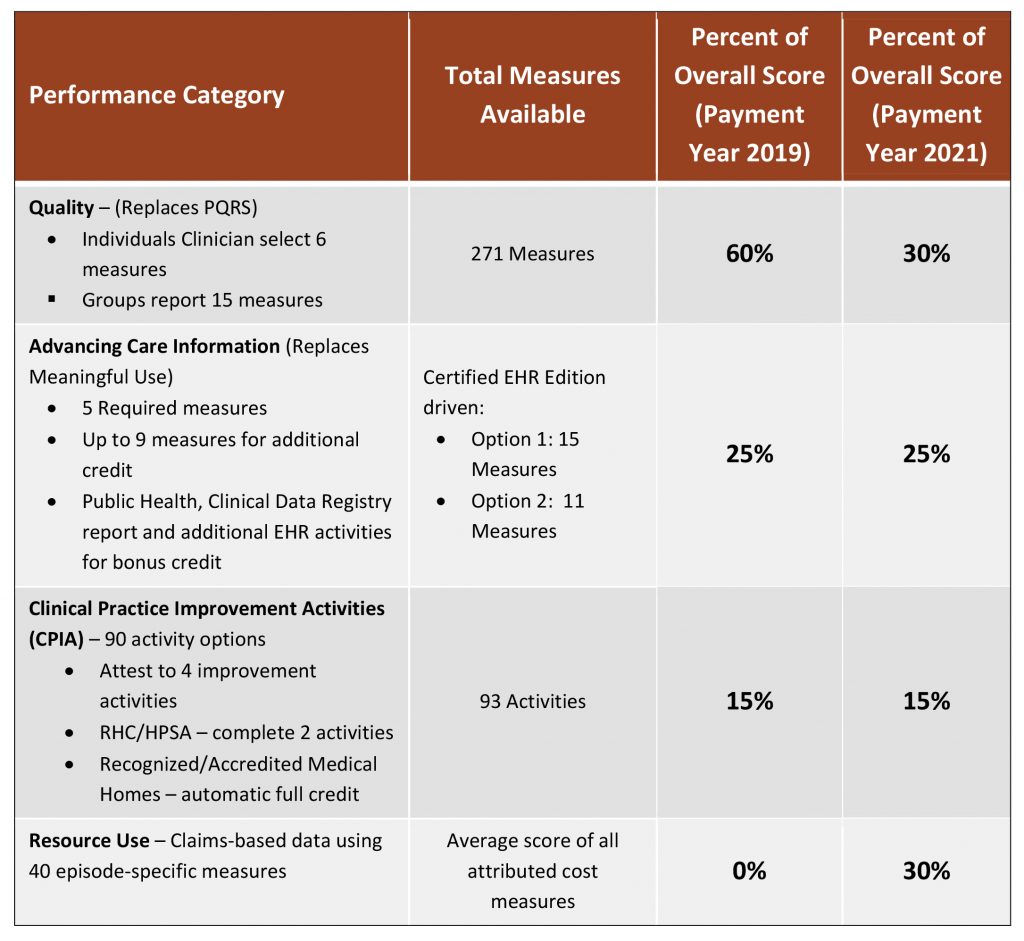
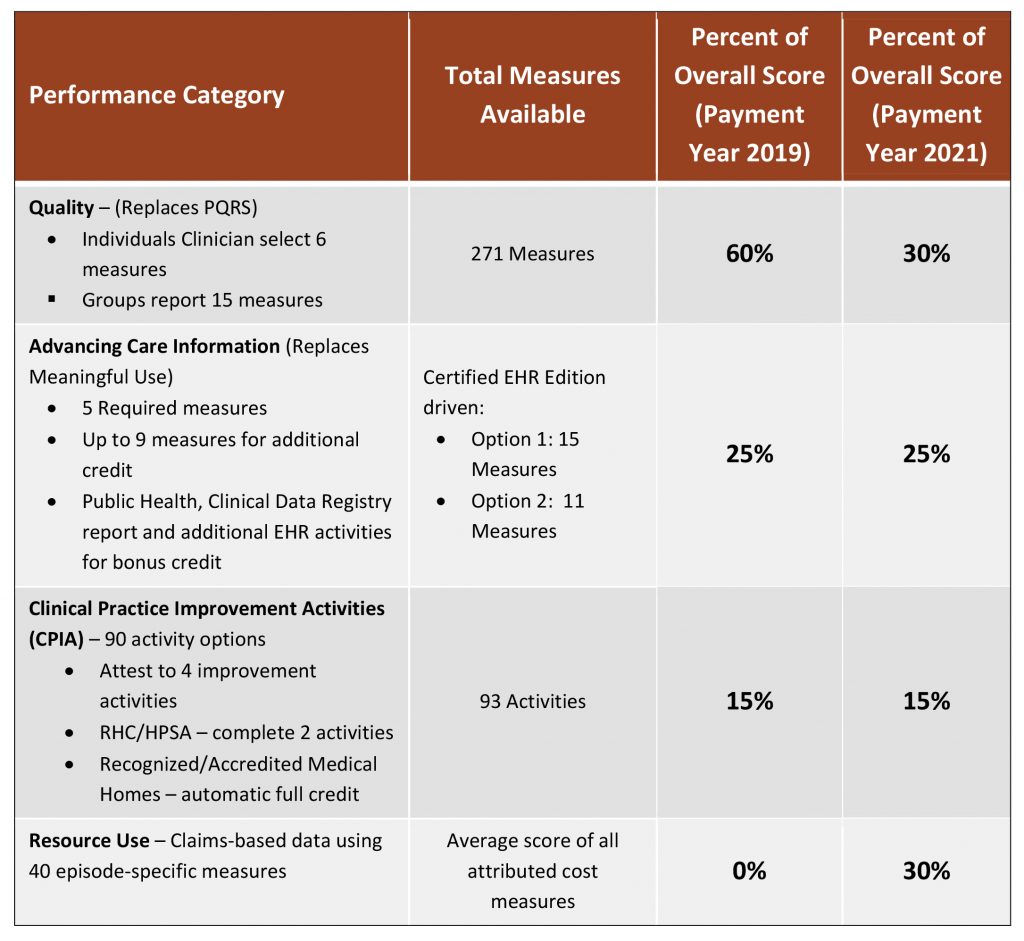
MIPS Scoring Explained
Given that nearly 90 percent of clinicians are expected to fall under a MIPS payment arrangement, it is important to understand how scoring will occur. Essentially, a single composite score for MIPS will be based on weighted performance in four categories: quality, cost, advancing care information, and clinical practice improvement activities (see Figure 3). Ultimately, MIPS rewards and penalties will be tied to a clinician’s composite performance score, and payment will wash from low-performing to high-performing providers in a budget-neutral fashion. Maximum points can be earned under the Clinical Practice Improvement Activities (CPIA) category for official medical home status under NCQA, The Joint Commission, URAC or AAAHC; or, NCQA patient-centered specialty practice (PCSP) achievement. Additionally, the formerly known CMS Electronic Health Records (EHR) Meaningful Use program is now represented under MIPS by the Advancing Care Information composite performance score category.
Where can I get help and learn more?
- CMS Quality Payment Program interactive website. Offers a practical overview of the new program and can assist in identifying appropriate measures and activities based on your specialty. Go to: https://qpp.cms.gov/
- atom Alliance and the Alabama Quality Assurance Foundation (AQAF). The CMS Quality Innovation Network (QIN)-Quality Improvement Organization (QIO) for Alabama that works on data-driven initiatives. Go to: http://atomalliance.org/
- CMS Innovation Center. Provides comprehensive information about alternative payment models being implemented and tested across the country. Go to: https://innovation.cms.gov/
Conclusion
A fundamental change is required to move from volume to value in payment for health care services. Today, much of health care economics is still functioning under Category 1, fee-for-service, but the roadmap towards value has been laid out under MACRA. Health care providers who understand the direction CMS is driving health care economics will be better positioned to work collaboratively with their community-based peers and payers as they move along this continuum. The stage is set for a new era of value in health care.
Sources
1 Federal Register. Medicare Program; Merit-Based Incentive Payment System (MIPS) and Alternative Payment Model (APM) Incentive Under the Physician Fee Schedule, and Criteria for Physician-Focused Payment Models. https://www.federalregister.gov/articles/2016/05/09/2016-10032/medicare-program-merit-based-incentive-payment-system-mips-and-alternative-payment-model-apm. Published May 9, 2016. Accessed August 12, 2016.
2 CMS. Quality Payment Program. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/MACRA-MIPS-and-APMs/NPRM-QPP-Fact-Sheet.pdf. Accessed August 25, 2016.
3 CMS. The CMS Blog, Plans for Quality Payment Program in 2017: Pick Your Pace. https://blog.cms.gov/2016/09/08/qualitypaymentprogram-pickyourpace/. Published September 8, 2016. Accessed September 12, 2016.
4 CMS. MACRA RFI Posting. https://innovation.cms.gov/Files/x/macra-faq.pdf. Accessed August 25, 2016.
5 CMS. The CMS Blog, Plans for Quality Payment Program in 2017: Pick Your Pace. https://blog.cms.gov/2016/09/08/qualitypaymentprogram-pickyourpace/. Published September 8, 2016. Accessed September 12, 2016.
6 CMS Proposed Rule, Medicare Program; Merit-Based Incentive Payment System (MIPS) and Alternative Payment Model (APM) Incentive under the Physician Fee Schedule, and Criteria for Physician-Focused Payment Models, https://www.gpo.gov/fdsys/pkg/FR-2016-05-09/pdf/2016-10032.pdf, Table 63. Published May 9, 2016. Accessed August 25, 2016.
7 Health Care Payment Learning & Action Network. Accelerating and Aligning Population-Based Payment Models: Data Sharing. https://hcp-lan.org/groups/pbp/ds-final-whitepaper/. Published August 8, 2016. Accessed August 12, 2016.
8 BlueCross BlueShield of Alabama. Quality Management Program. https://www.bcbsal.org/web/quality-initiatives.html. Accessed September 13, 2016.
9 CMS Innovation Center. Comprehensive Primary Care Plus. https://innovation.cms.gov/initiatives/comprehensive-primary-care-plus. Accessed September 13, 2016.
10 CMS. The CMS Blog, Plans for Quality Payment Program in 2017: Pick Your Pace. https://blog.cms.gov/2016/09/08/qualitypaymentprogram-pickyourpace/. Published September 8, 2016. Accessed September 12, 2016.
11 CMS. MIPS Scoring Methodology Overview. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/MACRA-MIPS-and-APMs/MIPS-Scoring-Methodology-slide-deck.pdf. Accessed August 25, 2016.

 Editorial contributed by John Meigs Jr., M.D., president of the American Academy of Family Physicians, member of the Medical Association Board of Censors, and a family physician in Centreville, Ala. Editorial reprinted by permission.
Editorial contributed by John Meigs Jr., M.D., president of the American Academy of Family Physicians, member of the Medical Association Board of Censors, and a family physician in Centreville, Ala. Editorial reprinted by permission.