It’s Not Just About Opioids…
According to the National Institute on Drug Abuse, more than 30 percent of overdoses in the United States involving opioids also involve benzodiazepines, or “benzos.” Statistics from the Centers for Disease Control and Prevention show more than 115 Americans die each day from an opioid-related overdose.
However, between 1996 and 2013 the number of adults who filled a benzodiazepine prescription increased by 67 percent from 8.1 million to 13.5 million. In 2015, 23 percent of people who died of an opioid-related overdose also tested positive for benzodiazepines.
In a study published in the British Medical Journal in March 2017 of more than 300,000 continuously insured patients receiving opioid prescriptions between 2001 and 2013, the percentage of persons also prescribed benzodiazepines rose to 17 percent in 2013 from nine percent in 2001. The study showed those concurrently using both drugs are at higher risk of visiting the emergency department or being admitted to a hospital for a drug-related emergency.
In March 2016, the CDC issued new guidelines for the prescribing of opioids, which included a recommendation to avoid prescribing benzodiazepines concurrently with opioids when possible. In October 2016, the Food and Drug Administration issued a “black box” warning for prescription opioids and benzodiazepines highlighting the dangers of administering these medications together. (See https://www.advisory.com/daily-briefing/2016/09/01/black-box-opioid-benzodiazepines)
Let’s talk about benzos.
As with all medications, benzodiazepines have their usefulness. If prescribed and taken correctly, this class of medications can be extraordinarily helpful to patients. Benzodiazepines calm or sedate a person by raising the level of the inhibitory neurotransmitter GABA in the brain. Common benzodiazepines include alprazolam (Xanax), diazepam (Valium) and clonazepam (Klonopin).
Alprazolam is the most prescribed benzodiazepine in Alabama, according to the Alabama Board of Medical Examiners.
“Benzodiazepines are very effective medications for the treatment of acute anxiety just as opioids are very useful for the treatment of acute pain. But also like opioids, benzodiazepines will cause the development of physiologic tolerance if used regularly, and this often causes a loss of therapeutic effect if the dose is not continuously escalated. For this reason, they are not ideal medications as the primary treatment of chronic anxiety,” said Luke Engeriser, M.D., Assistant Professor of Psychiatry at USA Health College of Medicine and Deputy Chief Medical Officer, AltaPointe Health Systems in Mobile. “Benzodiazepines are most useful when prescribed for brief periods when someone is going through a major crisis or exacerbation of symptoms, for example after the loss of a loved one. Ideally, regular use of the medication would only be for one or two weeks. We
also sometimes will use a benzodiazepine for a time-limited period when we are initiating an antidepressant medication like an SSRI or SNRI for treatment of chronic anxiety. Although these antidepressant medications are very effective for anxiety, it sometimes takes a few weeks before the medication has a sufficient therapeutic effect.”
Other physicians, like David Herrick, M.D., of Montgomery, agree with Dr. Engeriser that as physicians prescribe benzodiazepines, extra care should be taken in monitoring the patient.
“All medications have their place, but it’s the way they are used or misused that’s creating a deadly problem. While using opioids and benzos together is not completely forbidden, it is something that has to be done very, very carefully. Most people don’t have to be on benzodiazepines all the time. If the patient has a real anxiety disorder, then that patient should be under the care of a psychiatrist,” Dr. Herrick said. “Benzos are intended to be used for the short term. I think the medical community should consider benzodiazepines just as risky as opioids and monitor and treat their patients who are using them just as carefully as their patients who are taking opioids…with the same amount of care and concern.”
Going back to school.
According to Dr. Merrill Norton, PharmD., ICCDP-D, Clinical Associate Professor at the University of Georgia College of Pharmacy, although benzodiazepines have been in use since the 1950s, education about their proper use and potential harm has not kept up with the times.
“The problem with opioids and benzodiazepines, even at prescribed levels, is understanding which opioid interacts with which benzo?” Dr. Norton explained. “This is where the physician has to be very astute. What needs to happen now is a consistent training mechanism for physicians who prescribe buprenorphine, methadone, or have patients on these medications. What the benzo is doing is helping modify the anxiety that is being triggered by the opioid withdrawal. That’s why they use it. And this is why the physician needs to be better trained not only in the prescribing of the opioid but also with benzos and how they react to one another.”
Dr. Norton suggested before prescribing a benzodiazepine, physicians should evaluate the patient for tendencies to misuse drugs and/or alcohol or if the patient has a history of misuse. Depending on the complexity of the patient’s care needs, consultation or referral to an addiction medicine physician may be necessary. Certain aberrant behaviors also may be a feature in some patients who are prescribed benzodiazepines and may include diversion of valid prescriptions, illicit sale or use in manners alternate to the prescribed dosage, route and frequency.
“Physicians need to know that benzodiazepines are useful short term but have extreme dangers to medication safety to patients who are placed on long-term regimes. Physicians also need to be aware of each benzodiazepine medication’s half-life, tolerance curves, basic pharmacodynamics and pharmacokinetic properties of each, and how to identify and manage benzodiazepine withdrawal when it occurs. Basically, physicians need to re-educate themselves on these medications. I’m finding that most physicians are already very cautious when it comes to prescribing benzodiazepines, but I don’t know how aware they are of the many types of drug interactions that can happen,” Dr. Norton said.
The Medical Association will again offer three live Prescribing and Pharmacology of Controlled Drugs courses in 2019. Drs. Engeriser, Herrick and Norton have all participated in these lectures in the past as guest faculty members and stress the importance of presenting evidence-based information and case studies to the attendees. The courses in 2019 will be March 2-3 in Auburn, Aug. 2-4 in Destin, and Nov. 23-24 in Birmingham. More information about specific topics and faculty will be available from the Association’s Education Department at a later date.
The Medical Association recently unveiled its new online OnDemand Education Center, which includes seven Alabama Opioid Prescribing courses that meet the Alabama Board of Medical Examiners’ requirements for holders of an ASCS and are free to members. One course specifically deals with benzodiazepines: Use and Misuse of Benzodiazepines.
What tools can physicians use to avoid potentially deadly medication interactions?
There are many tools physicians can use to help screen their patients for a history of alcohol and/or drug addiction before prescribing benzodiazepines. Physicians agree that adding a benzodiazepine into the mix of medications for a patient who has a history of addiction may only be adding fuel to the fire.
“Prescribing a benzodiazepine to a patient with a history of addiction to other substances increases the risk that a patient could develop an addiction to benzodiazepines or that the benzodiazepine could trigger a relapse on the drug of choice. When prescribing any controlled substance, we should also regularly check the PDMP,” explained Dr. Engeriser.
The Prescription Drug Monitoring Program was developed to promote the public health and welfare by detecting diversion, abuse and misuse of prescription medications classified as controlled substances under the Alabama Uniform Controlled Substances Act. Under the Code of Alabama, 1975, § 20-2-210, et seq., the Alabama Department of Public Health was authorized to establish, create and maintain a controlled substances prescription database program. This law requires anyone who dispenses Class II, III, IV, V controlled substances to report daily the dispensing of these drugs to the database. For more information about the Alabama PDMP, or to set up an account, log on here: http://alabamapublichealth.gov/pdmp/
Another helpful tool Dr. Norton suggested physicians can have at their fingertips to help spot bad drug interactions is the app, UpToDate. This app is one of the fastest apps physicians can use to double-check for drug interactions as they are writing prescriptions. It is, however, a subscription service, but the app comes with clinical decision support with evidence-based clinical information, including drug topics and recommendations. To learn more about UpToDate, services, subscription options, and how to download the app for your mobile device or EHR, log on here: https://www.uptodate.com/home/why-uptodate
Medical Association members can also subscribe to The Medical Letter on Drugs and Therapeutics at a reduced rate. The Medical Letter is a biweekly publication that provides evidence-based, peer-reviewed evaluations of new FDA-approved drugs with conclusions reached by a consensus of experts; new information on previously approved drugs including pivotal clinical trials, new indications, and safety warnings; consensus recommendations for
the preferred and alternative treatments for common disorders; and comparative reviews of drugs for a given indication with particular attention to clinical efficacy, adverse effects, drug interactions, and cost. A subscription includes online and print access, a mobile app, and CME opportunities. To learn more about The Medical Letter, log on here: https://bit.ly/2Jj2EwW
What’s next?
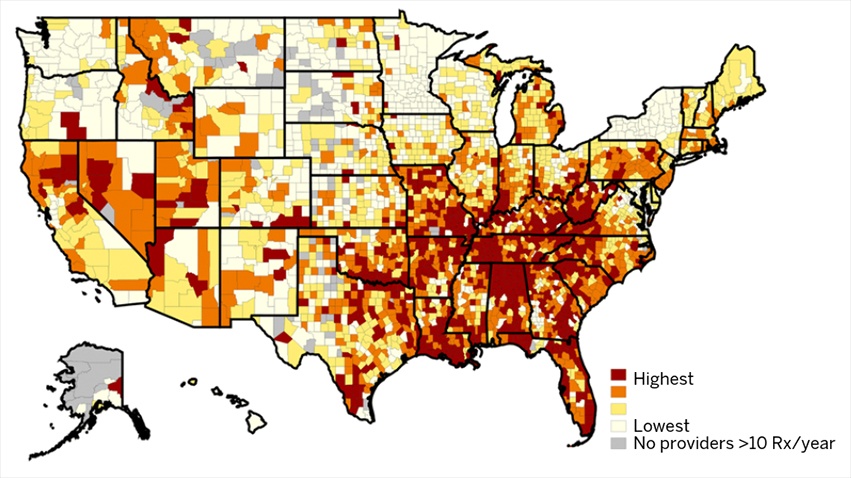
A new study by the University of Michigan and published in the Journal of General Internal Medicine maps out county-by-county the prescribing habits of benzodiazepines. The South ranks at the top of the spectrum.
The study is based on data about all prescriptions written in 2015 by primary care providers for patients in the Medicare Part D prescription drug program. The researchers combined that information with county-level health and socioeconomic data from the County Health Rankings project, a project of the Robert Wood Johnson Foundation and the University of Wisconsin.
In the single year studied, the 122,054 primary care providers included in the study prescribed 728 million days’ worth of benzodiazepines to their patients, at a cost of $200 million.
The states with the highest intensity of prescribing — which the researchers defined as prescription days of benzodiazepines relative to all prescribed medication days — were Alabama, Tennessee, West Virginia, Florida and Louisiana. States with the lowest intensity were Minnesota, Alaska, New
York, Hawaii and South Dakota. Across all types of providers, primary care and otherwise, benzodiazepines accounted for 2.3 percent of all medication days prescribed to Part D participants by those providers that year.
Physicians agree it’s time to take another look at these medications.
“Benzos have as many problems as opioids do — they are addictive, sedating and deadly if they are not prescribed and used properly.” Dr. Herrick said. “We as physicians need to be more aware of these dangers and treat benzos the way we treat opioids with a lot more respect than we are right now. If you write the prescription and sign your name to it, you had better understand what you’re writing before you hand it off to your patient because it could cost that patient his life. We have gotten a bit cavalier about how we prescribe benzos, and we need to take a look at how and why we prescribe them. This is a real issue, and we need to take it more seriously. It’s time we take a hard look at how these are prescribed and why.”
Dr. Engeriser, however, offered a word of caution. Where physicians who prescribe opioids may have instinctively wanted to stop prescribing them altogether as the national epidemic was on the rise that cannot be the case with benzodiazepines.
“As providers become more careful about prescribing practices, there will likely be an increase in the desire to stop using benzodiazepines for certain patients. Benzodiazepine withdrawal is similar to alcohol withdrawal and can lead to seizures, delirium tremens, and death. For that reason, it is critical that patients not have their benzodiazepines abruptly stopped. There are different strategies for the tapering of benzodiazepines. The important thing in the outpatient setting is to taper the benzodiazepine slowly enough that severe withdrawal symptoms do not emerge. This is often done more easily with a benzodiazepine with a longer half-life such as clonazepam than a shorter half-life like alprazolam. On an inpatient unit, benzodiazepine taper can be more rapid, using as needed benzodiazepines to treat emergent withdrawal, with dosing guided by a scale, such as the Clinical Institute Withdrawal Assessment for Alcohol-Revised (CIWA-Ar).” Dr. Engeriser said.
Posted in: Opioid
Leave a Comment (0) →


 The states with the highest intensity of prescribing — which the researchers defined as prescription days of benzodiazepines relative to all prescribed medication days — were Alabama, Tennessee, West Virginia, Florida and Louisiana.
The states with the highest intensity of prescribing — which the researchers defined as prescription days of benzodiazepines relative to all prescribed medication days — were Alabama, Tennessee, West Virginia, Florida and Louisiana.