Posted by Christina Flack on June 7, 2019
In times of illness, injury, and emergency, patients depend on their physicians. But what if no one was on call? Public health would be in jeopardy. The same holds true for organized medicine when the legislature is in session.
If the Association had not been on call for its members, numerous inappropriate expansions to the scopes of practice for non-physicians would have passed; lawsuit opportunities against physicians would have increased; and poorly thought out “solutions” to the opioid abuse epidemic could have become law.
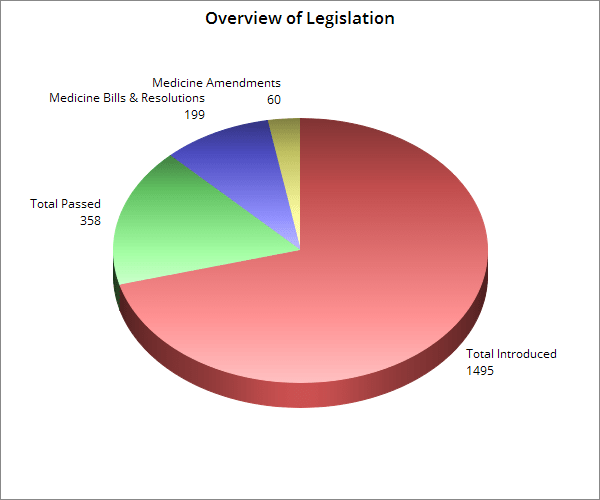
Overview of Legislation
[supsystic-tables id=2]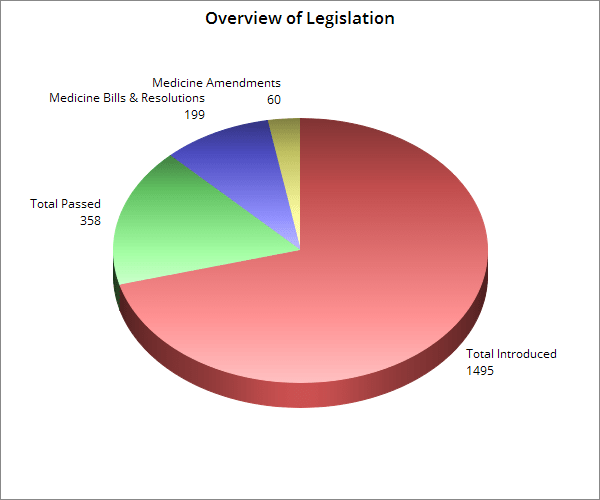
Moving Medicine Forward
The 2019 Legislative Session is over. For our advocacy efforts to remain successful moving forward, between now and the 2020 Session, the Association will be visiting with physicians and legislators around the state to ensure the views of medicine continue to be heard. Visit our Advocacy Portal to find out how you can get involved.
If no one was on call . . . legislation setting up a process for establishing guidelines for prescription of buprenorphine in nonresidential treatment programs would not have passed. The Association worked alongside the bill’s sponsor, Sen. Larry Stutts, M.D., in supporting this legislation and giving BME the authority to issue regulations on medication assisted treatment. The bill currently awaits the governor’s signature.
If no one was on call . . . the importance of updating statewide immunization registry requirements would not have received the exposure it did. The Association worked with Sen. Tim Melson, M.D. and the Department of Public Health on SB256. The bill was set for final passage in the House, but it unfortunately did not receive a vote on the final day of the session. The Association will support the bill again moving forward.
If no one was on call . . . “truth in advertising” legislation would not have been brought forward. The Association assisted Sen. Tim Melson, M.D. on the legislation to prohibit deceptive or misleading advertising and require all health professionals to take steps to inform patients of their certifications. Although the bill did not receive a vote for final passage, it remains a priority for the Association per a 2018 House of Delegates Resolution.
If no one was on call . . . the rural physician tax credit would not have been introduced and support for this bill would not have grown. SB374 would have amended the current definition of rural, strengthened the residency requirement, and extended the tax credit from 5 to 6 years. The tax credit is a significant factor in physician retention in Alabama’s rural communities and, while it did not pass, it remains a priority for the Association.
If no one was on call . . . the Board of Medical Scholarship Awards may have been consolidated into some other state agency or seen its funding eliminated. The Association worked with BMSA to request additional funding for this highly successful program, but the increase was ultimately not included in the budget. Like the Rural Physician Tax Credit, the BMSA is a critical tool to placing physicians in rural areas and the Association will continue pushing increased BMSA funding moving forward.
If no one was on call . . . the upgrades that transformed the PDMP into a more user-friendly and valuable tool for physicians may not have continued to be funded. The Association supports maintaining the increased appropriations for the PDMP.
Scope Creep – Replacing Education with Legislation
Everyone wants to be a physician, but few are willing to endure medical school, residency, and all the other various education and training requirements to become an M.D. or D.O. Instead of pursuing higher education, non-physicians are pursuing legislative changes as a means to practice medicine. The Association opposes any scope of practice expansions that could endanger quality care for patients.
If no one was on call . . . the physician referral requirement for physical therapy would have been abolished. Patients would not receive a medical diagnosis, potentially receive unnecessary care, and could be delayed in obtaining appropriate care. In conjunction with the Alabama Orthopaedic Society and other allied specialties, the Medical Association convinced members of the Senate Health Committee to uphold the importance of a diagnosis and vote down SB25, 8-2. This bill is expected to return in 2020.
If no one was on call . . . safety standards for anesthesia care would have been significantly lowered. In addition to abolishing physician direction of CRNAs, SB156 could have also led to CRNA prescribing with no physician oversight. In conjunction with the Alabama State Society of Anesthesiologists and other allied specialty societies, the Medical Association convinced legislators not to support the legislation and it failed without receiving a vote. This bill is expected to return in 2020.
If no one was on call . . . optometrists could have begun performing eye surgeries using scalpels and lasers. Moreover, SB114 would have given the Alabama Board of Optometry the sole power to define what is considered to be the practice of optometry simply by regulation. Ultimately, the bill did not receive a vote in committee due to the work of the Alabama Academy of Ophthalmology, other allied specialty societies, and the Medical Association. This bill is expected to return in 2020.
If no one was on call . . . a new state board with unprecedented authority over radiation and medical imaging could have been created. Among other things, SB165 would have allowed this new board to determine scopes of practice for x-ray operators, radiation therapists, radiographers, radiologist assistants, magnetic resonance technologists, and nuclear medicine technologists (to name a few). This bill could have increased costs for medical practices and dangerously expanded the scopes of practice for non-physicians. While the bill did not receive a vote in committee, it is expected to return in 2020.
If no one was on call . . . all podiatrists would have been granted the ability to perform surgery on the ankle and lower leg. HB310 significantly expanded the scope of practice of podiatrists, who only 10 years ago standardized their residency programs nationwide. This legislation failed to receive a vote in committee, but, similar to the other “scope creep” pieces of legislation, the bill is expected to return in 2020.
If no one was on call . . . physician collaborative practice with nurses could have been abolished. Under the legislation passed this session, nurses are now allowed to apply for a multistate license through a compact. Previous nursing compact legislation, however, had attempted to allow other states’ laws to be substituted for Alabama’s. The Association worked to ensure nothing in this bill alters current collaborative practice agreements.
Beating Back the Lawsuit Industry
Plaintiff trial lawyers are constantly seeking new opportunities to sue doctors. Alabama’s medical liability laws have long been recognized for ensuring a stable legal climate and fostering fairness in the courtroom. Yet, year after year, personal injury lawyers seek to undo those laws and allow more frivolous lawsuits to be filed against physicians.
If no one was on call . . . multiple bills dictating standards of care and increasing lawsuits against physicians may have passed. For instance, physicians could have faced lawsuits and criminal penalties if a patient overdosed as a result of an opioid prescription. Also, physicians participating in a state authorized needle exchange program aimed at curbing the spread of disease via IV drug use would not have received proper liability protections. None of the language proposed by plaintiff lawyers passed into law.
If no one was on call . . . plaintiff lawyer-drafted legislation concerning involuntary commitment procedures would have created new lawsuit opportunities against physicians. These 6 different pieces of legislation amend current law to allow a nurse practitioner or physician assistant to coordinate with a physician in deciding to treat an individual who is unable to consent and without having to first attempt to contact a family member. Before passing, however, the Association successfully added much-needed liability protection for physicians to these bills.
If no one was on call . . . physicians administering chemical castration drugs to certain inmates would not have been shielded from liability. The Association worked with the bill sponsor to add language protecting physicians who administer these drugs to those individuals convicted of sexual offenses against children age 13 and under who opt to take the medication as a condition of parole.
If no one was on call . . . support would not have grown for legislation increasing penalties on attorneys who encourage lawsuits. HB181 would strengthen existing criminal and civil penalties on attorneys who give, offer, or promise valuable consideration to a potential client as an inducement to file a lawsuit. The bill passed committee but never received a final vote.
On the Prescribing Front
This session, many bills regarding prescribing practices and prescription drugs were introduced. Some of this legislation was pitched as improving access to quality care, but were actually back-door “scope creep” bills.
If no one was on call . . . Alabama’s existing prescription authorization law would have been repealed, endangering patients and creating hassles and expenses for physicians. Prior to revisions negotiated by the Association, the legislation would have given pharmacists the default ability to substitute drugs and could have allowed the Board of Pharmacy to issue regulations affecting physician prescribing practices. This language was successfully removed by the Association before the bill passed. Physician authority in issuing prescriptions is unchanged.
If no one was on call . . . poorly-written legislation could have passed on biologic substitution, delaying patient and physician notification. The Association negotiated language requiring pharmacists to communicate an authorized substitution within 24 hours to the physician and patient. The notification to physicians must be made via phone or fax or the e-prescribe software used by the physician. The bill that passed was supported by the Medical Association.
If no one was on call . . . legislation opening the door for widespread prosecution of physicians prescribing opioids could have become law. The legislation was successfully amended to adopt the federal standard that all prescribers and pharmacists are currently held to by the DEA. As passed, only someone who issues a prescription knowingly or intentionally for other than a legitimate medical purpose and outside the usual course of his or her practice may be charged.
If no one was on call . . . arbitrary physician requirements for prescribing controlled substances could have been enacted. Working with proponents of the bill, the Association sought to change the bill and default to existing medical regulations governing controlled substance prescribing practices. The legislation, however, did not pass.
Other Legislation of Interest
Medical Marijuana . . . having undergone significant changes as it moved through the legislature, this bill now reauthorizes CBD research at UAB via “Carly’s Law” and creates a study commission to make recommendations to the Legislature relating to medical use of cannabis in Alabama. The Commission will be comprised of 15 members and will issue its findings and draft legislation by December 1, 2019.
Abortion . . . this legislation criminalizes the performing of an abortion or attempted abortion, with exceptions for instances where the physical and mental health of the mother is at risk and for treatment of ectopic and cornu implantations. The sole purpose of the bill is to challenge the United States Supreme Court’s prior rulings on abortion laws and a lawsuit has already been filed asking a judge to block its implementation.
Pharmacist/Physician Collaborative Practice . . . this legislation allows pharmacists and physicians to voluntarily enter into agreements for medication management services. Unlike collaborative practice laws of other states, HB35 does not specify what types of authority or activities a physician may delegate to a pharmacist. For example, HB35 does not state that ultimate determinations regarding patient care rest with the physician. Moreover, HB35 does not require pharmacists to input information into patients’ medical records if dosage strength or medication type is changed. HB35 also does not prohibit pharmacists from prescribing any drugs – including controlled substances – and does not prohibit pharmacists from ordering lab tests. Despite patient safety and public health concerns raised by the Association, the bill was passed and signed into law. The Alabama Board of Pharmacy and the Alabama Board of Medical Examiners are now responsible for promulgating rules to enforce the act.
Human Trafficking . . . multiples bills introduced this session would have set new human trafficking training requirements and standards of care for physicians. The failure of a physician to follow these new guidelines could have effectively created liability. In the end, the bills were changed into resolutions calling for education and training which received widespread support.
Gunshot Wound Reporting . . . as introduced, these bills mandated physicians to report all patients receiving treatment for gunshot wounds or acts of violence and contained no language protecting reporting physicians from liability. The Association worked to successfully amend this legislation to limit its scope to only gunshots and provide protection for physicians.
Genetic Counselors . . . these bills would have created an entirely new board authorized to establish regulations for genetic counselors and genetic counseling in Alabama. Working with bill proponents, the Association exempted physicians from regulation under the act and specified that genetic counselors are not authorized to practice medicine. The bill did not pass.
Using Cell Phones While Driving . . . prior to the Association’s successful addition of an amendment, this bill would have outright prohibited the use of cell phones while driving, including physicians responding to an emergency situation. Ultimately, the bill did not pass, even with the Association’s amendment.
General Fund Appropriations . . . in addition to funding for the PDMP mentioned above, the general fund budget contained other appropriations for various health causes. Specifically, $200,000 will be expended for the Addiction Prevention Coalition; $100,000 for the Amyotrophic Lateral Sclerosis (ALS) Association; and $500,000 for the Breast and Cervical Cancer Early Detection Program. Also, the CHIP program received full funding; and there are no scheduled cuts to physician payments in next year’s Medicaid budget.