Category: Members
-
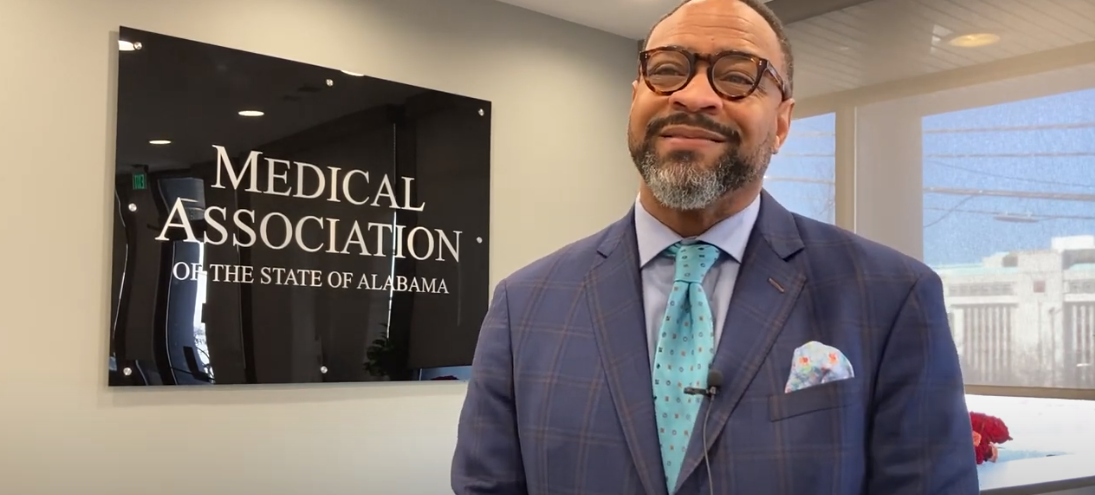
Gov. Ivey Declares March 30 “Doctors Day” in Alabama, Doctors Share Stories of Why They Became Physicians
Gov. Kay Ivey has proclaimed March 30 as “Doctors Day” in Alabama and doctors are celebrating the occasion by sharing personal stories about why they chose medicine for their profession. In a video released by the Medical Association of the State of Alabama, several doctors say as they were growing up it was their own doctors who…
-
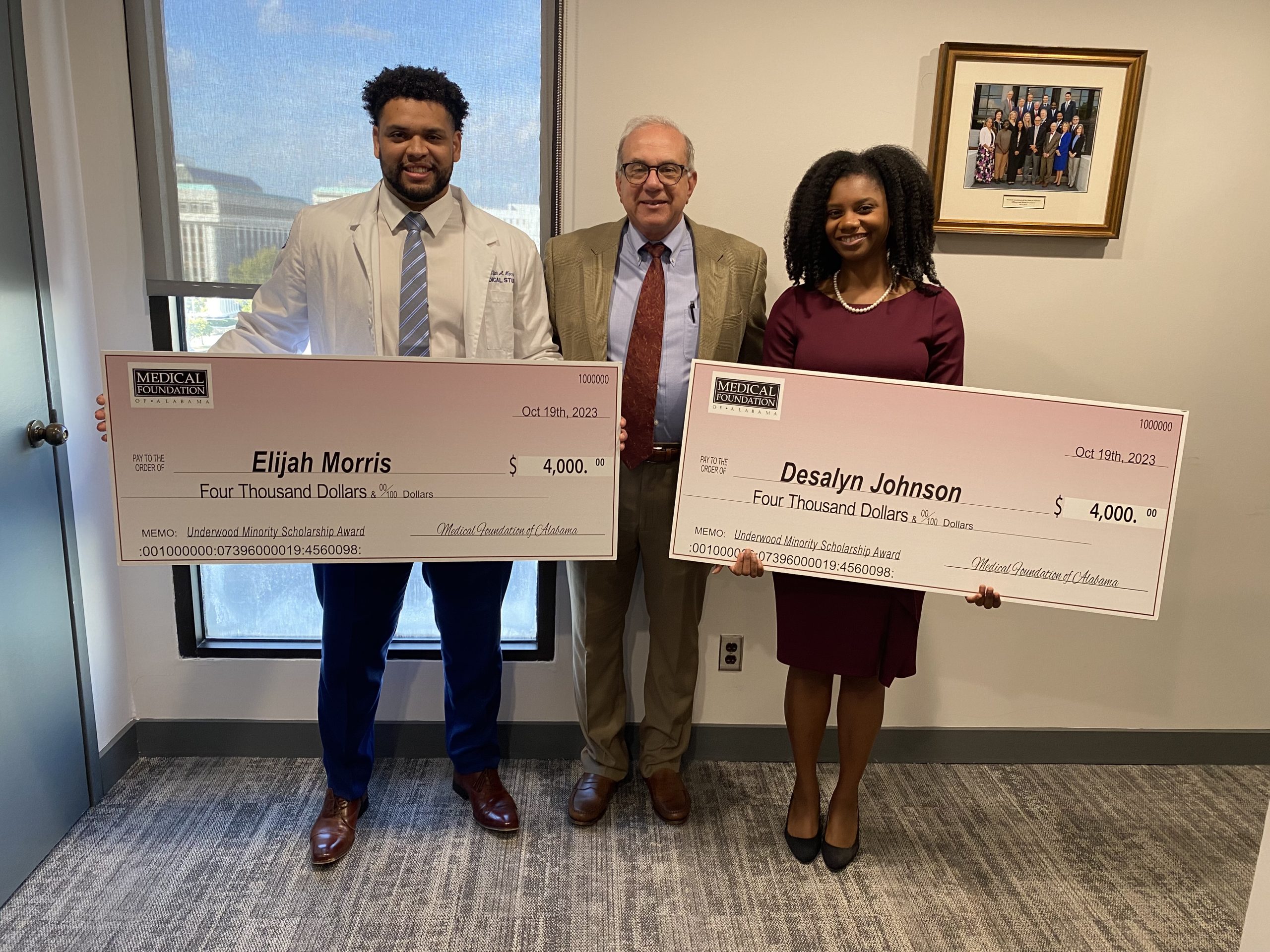
Medical Association Awards Two Students with Underwood Minority Scholarships
The Medical Association of the State of Alabama awarded two $4,000 scholarships to minority medical students Desalyn Johnson and Elijah Morris to help pay the cost of medical school. The Underwood Minority Scholarship Award is named in honor of Dr. Jefferson Underwood, III, a Montgomery physician who was the first African-American man to serve as the Association’s president. African-American students who are…
-
Payor Auditing Activities
By: Kelli Carpenter Fleming During the height of the COVID-19 pandemic, the Centers for Medicare & Medicaid Services (“CMS”) suspended certain payor audit and oversight activities. However, now that communities are beginning to reopen, so are the audit activities. CMS and other third-party payors are increasing their audit activities, including claims filed during the public…
-
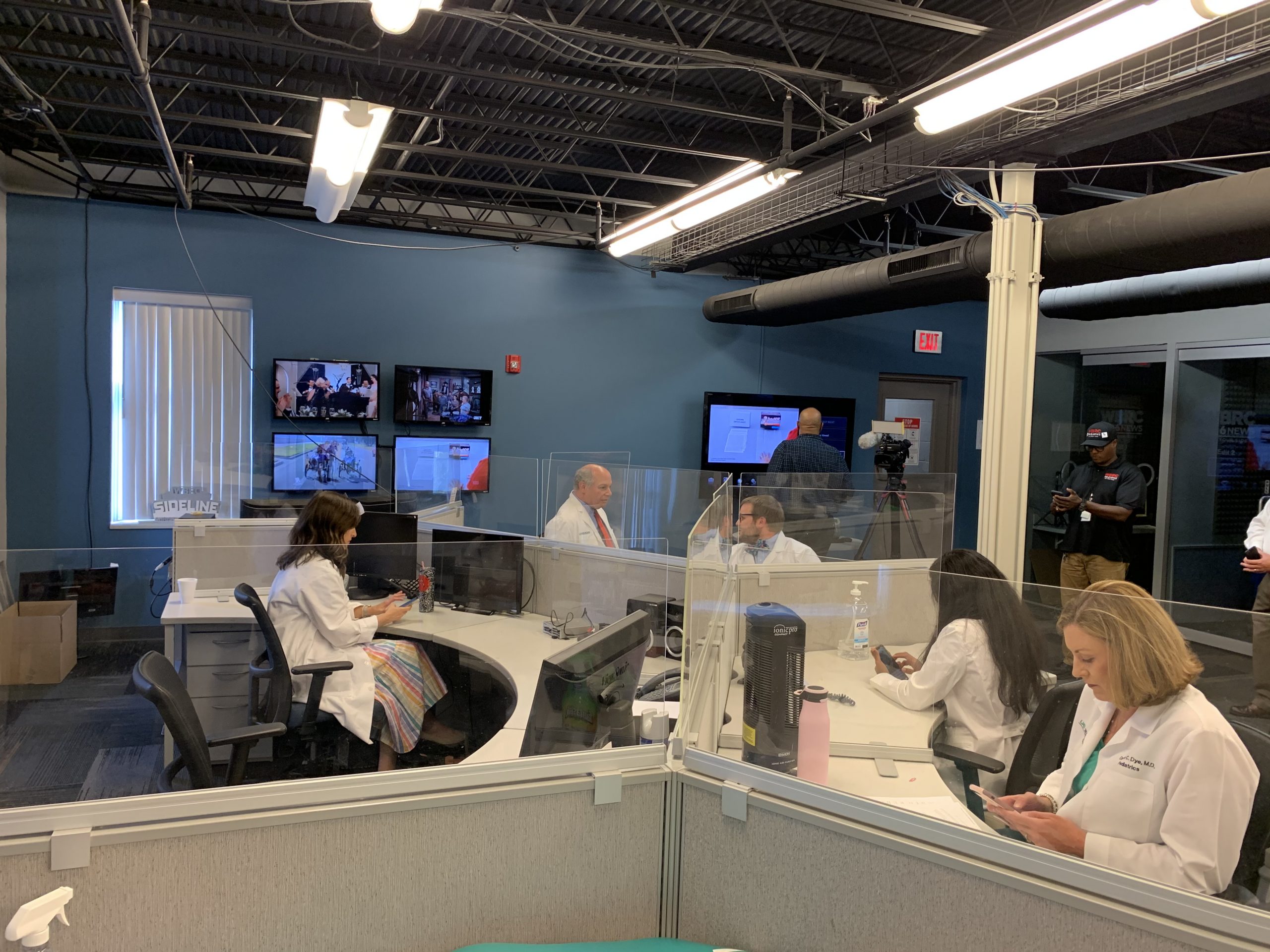
Alabama Doctors Host Two Telethons to Answer Viewers’ Questions About COVID-19 Vaccines
Last Thursday, doctors with the Medical Association of the State of Alabama and the Alabama Chapter of the American Academy of Pediatrics answered questions from over 200 callers about the safety and effectiveness of COVID-19 vaccines during newscasts on WBRC Fox 6. Yesterday another group of our physicians went live on air with WKRG in…
-

No Honor Among Thieves
Most Americans will likely never forget where they were in March of 2020 when the world seemingly shut down. While many used that time to reflect, enjoyed down time with family or even binge watched streaming services, health care workers geared up to save the lives of people impacted by COVID-19. The novelty of this…
-
Medical Association Supports Continued Funding for Maternal Death Investigations
‘Shocking’ Nearly 70% of Deaths Are Preventable, Experts Say MONTGOMERY – The Medical Association of the State of Alabama today joined Alabama legislators in calling for continued state funding to investigate why Alabama mothers die from childbirth and pregnancy complications at more than double the rate of women nationally. The funding for this research,…
-
Physician Recruitment Agreements – What You Need to Know
by Howard E. Bogard Both the federal Anti-kickback Statute and the Stark Law allow a hospital to provide certain financial assistance to aid a medical practice in its efforts to recruit and hire a new physician. Financial assistance can take many forms, including a collection guarantee, net income guarantee and/or payments with respect to a…
-
Partnering with ALAHA to Celebrate 2021 Doctors’ Day
Today is a day set aside nationwide to honor the physicians who care for us every day of the year. Doctors’ Day was established on March 30 in 1934, and later in 1991, President George H.W. Bush proclaimed National Doctors’ Day as a time for the nation to celebrate the dedication and leadership of physicians. …
-
Op-ed: Alabama physicians face challenges head-on during vaccine rollout
By: John Meigs, Jr., MD, President – Medical Association of the State of Alabama Because of a seemingly slow rollout of the COVID-19 vaccine, physicians have started to hear many concerns from their patients. Understandably, the people of Alabama are growing more eager each day to get vaccinated. Physicians were privileged to be included in…
-
