Month: December 2017
-

Alabama Experiences Significant Influenza Activity this Season
Influenza activity levels are increasing across the State of Alabama. Several positive influenza specimens in northern Alabama have been identified in the previous three weeks. While the flu season is just getting started in much of the country, activity is already high in Alabama. Flu is a very contagious respiratory illness. Some of the symptoms…
-

An Overlooked Epidemic: Older Americans Taking Too Many Unneeded Drugs
Consider it America’s other prescription drug epidemic. For decades, experts have warned that older Americans are taking too many unnecessary drugs, often prescribed by multiple doctors, for dubious or unknown reasons. Researchers estimate that 25 percent of people ages 65 to 69 take at least five prescription drugs to treat chronic conditions, a figure that jumps to nearly…
-

Medical Association Works to Ease MOC Frustrations
Frustrations with the current Maintenance of Certification process brought together Medical Association Executive Director Mark Jackson and Council on Medical Service member Jeff Rickert, M.D., and representatives from other state medical societies and individual specialty boards for a series of meetings with the American Board of Medical Specialties. The daylong meeting in Chicago was called at the…
-

Medical Association’s 2018 State and Federal Agendas
The Medical Association Board of Censors has met and approved the Association’s 2018 State and Federal Agendas. These agendas were developed with guidance from the House of Delegates and input from individual physicians. As the Alabama Legislature and U.S. Congress begin their work for 2018, additional items affecting physicians, medical practices and patients may be…
-

Organized Medicine: Why Physician Membership is More Important Now than Ever Before.
“There’s strength in numbers” is a saying we all know well. Whereas one person can say something, it becomes a much more powerful display when more people join together in support or protest. In the past, it was not unusual for physicians to be members of their county medical society, specialty society, state medical association,…
-

HIPAA and the Holidays
As the holiday season builds momentum we are faced with numerous distractions like holiday decorations, taking advantage of online sales and soaking in the traditions that we look forward to each year. But this season of joy and giving should also be met with a heightened sense of awareness and adherence to HIPAA policies and…
-

AG Steve Marshall Speaks at November Education Weekend
BIRMINGHAM – Alabama Attorney General Steve Marshall addressed attendees during the Association’s Annual Medical Ethics seminar on Friday, Nov. 17, at the Hyatt Regency Hotel in Birmingham and helped kick off one of the largest weekends of educational offerings the Association has hosted since 2014. The weekend began on Friday, Nov. 17, with Ensuring Quality…
-
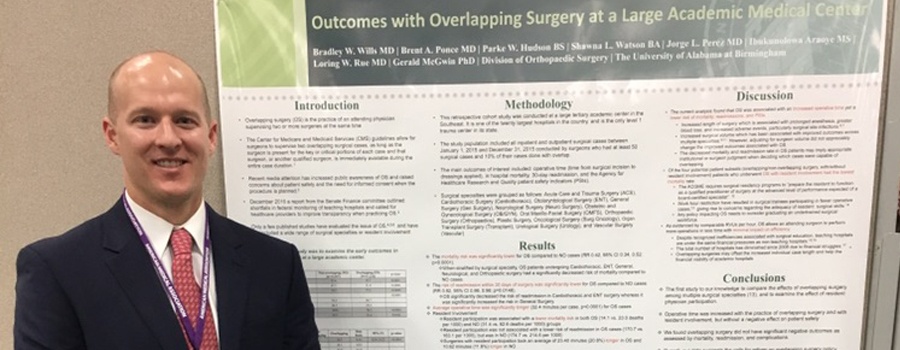
Annual Session Poster Symposium Winner Presents in Hawaii…and Wins!
Dr. Bradley Wills, who originally received first place at the Medical Association’s Second Annual Poster Symposium in April for his poster entitled Outcomes with Overlapping Surgery at a Large Academic Medical Center, presented his research poster at the 2017 AMA Interim Meeting in Honolulu in November and won the Resident-Fellow Section Division for Clinical Medicine.…