Posted by admin on December 11, 2017
“There’s strength in numbers” is a saying we all know well. Whereas one person can say something, it becomes a much more powerful display when more people join together in support or protest.
In the past, it was not unusual for physicians to be members of their county medical society, specialty society, state medical association, national specialty society, and national medical association, but these days those numbers are waning. When the practice of medicine seems to be changing almost daily, support for organized medicine as a whole seems to be dropping during a time at which patients and their physicians need help more than ever before.
The 2016 Survey of America’s Physicians: Practice Patterns & Perspectives conducted on behalf of The Physicians Foundation by Merritt Hawkins, captured a snapshot of what the nation’s physicians think about the state of medical care today. Some of the findings were enlightening.
- 80 percent of physicians are at capacity or have no time to see new patients
- 49 percent of physicians often have feelings of burnout
- 28 percent of physicians are only somewhat unfamiliar with MACRA
- 49 percent of physicians would not recommend a career in medicine
- 42 percent of physicians agree that EHRs have either reduced or detracted from their ability to deliver quality care
Ideally, physician membership in organized medicine would increase during difficult times facing the House of Medicine – times in which medicine is facing more intrusion by government regulation and restriction on how physicians can and do practice medicine, and the protection of patients’ rights. However, it would seem more physicians are moving away from the strength-in-numbers unified front that organized medicine provides to policymakers and replacing it with conflicting voices.
For example, in the 1950s, about 75 percent of all practicing physicians in the United States were members of the American Medical Association. According to a December 2016 article by Mother Jones online, its membership now is representative of about one-sixth of the nation’s physicians. So, where are all the physicians going?
What is the role of organized medicine?
Organized medicine groups are groups of physicians categorized into physician, young physician, resident and medical student sections. Each section works together to advocate collectively on behalf of the physician-patient relationship, patients’ rights, and medicine as a whole, but then each individual group works together to advocate for their section’s interests.
Giving physicians and medical students a voice in the business of medicine allows physicians to advocate for the best quality of care for their patients and ensures physicians are also treated fairly on the state and national levels.
In some cases, many young physicians may not even know about options to join organizations such as the AMA, the Medical Association, or even their local county medical society until the organization reaches out to them or a colleague mentions it. In Dr. Amber Clark’s case, it was a trip to an AMA meeting in Chicago that opened her eyes to the potential for organized medicine.
Dr. Amber Clark, who is in her second year of residency training in Physical Medicine and Rehabilitation at the University of Alabama at Birmingham School of Medicine, knew she wanted to be a physician since she was a little girl watching her pharmacist mother interact with her customers. But, even back then she knew she wanted more from her chosen profession.
“I always wanted that one-on-one relationship with patients, but (going to) Chicago introduced me to this concept of how we can make changes on more than just an individual basis but a population basis. That’s meaningful change!” Dr. Clark said. “It really is the responsibility of the physician, whether you’re in medical school or still in training or have completed your residency, to be a voice for yourself and your patient. Yes, we’re going to have more members that are going to be more vocal, that’s just the nature of life, but it’s still important to be one of those speaking out and being heard.”
Dr. Clark’s trip to Chicago was “mind-blowing,” allowing her to serve as an alternate delegate for the first time. Because the AMA trip to Chicago was her first introduction to organized medicine on a national stage, she did not know what to expect, which made for an even better experience.
“You have this collegiality of residents from all different walks of life and all different types of programs all coming together for one specific cause. We’re all advocating on behalf of our patients, but we’re also advocating on behalf of ourselves. There are so many other things that go on during these meetings behind the scenes that many physicians don’t know about because they don’t attend, but you assume people are advocating on your behalf. You can’t ever assume someone is fighting for you. You have to be willing to speak up. It just makes sense to participate,” Dr. Clark said.
Staying connected.
Across the country, organized medicine is having difficulty attracting and keeping members. As state and national membership organizations continue to add member benefits to entice members to stay connected, the number of physicians who are leaving the larger organizations for the smaller specialty societies seems to be increasing.
While there are still benefits of joining specialty societies, the larger membership organizations are left feeling the blow in their ranks…which means less bargaining power when it comes to negotiating on behalf of medicine.
Dr. Conrad Pierce has seen firsthand the power that comes with large membership organizations. He has seen it work well…and he has seen how it can fall apart when the members of the organization cannot manage its collective bargaining power.
About a year after he retired, Dr. Pierce began working for then-Sen. Jeff Sessions as a health care policy advisor when the Affordable Care Act was making its way through Congress. It was an arduous job trying to understand the proposed legislation, but condensing it down for someone not in medicine to understand was just as difficult.
“Legislators don’t know or understand much about medicine,” Dr. Pierce explained. “We all have to admit what we don’t know. Physicians know about medicine, so it only makes sense for physicians to be the ones to inform our policymakers about health care. Physicians are on the health care battle lines, out there taking care of their patients, helping them make those decisions that are truly life or death decisions for their families. Physicians have clout when we talk to our legislators. We can make them understand, in simple terms, the most complex issues in medicine. We do this every day when we discuss medical situations with our patients. If I have a patient with cancer, I can discuss that situation with my patient and explain the prognosis and treatment options. So, I should be able to discuss exactly why something in a proposed piece of legislation is either very good or very bad and how it will affect my patients and my practice. If we as physicians cannot talk to our legislators about medicine, where do you think they are going to get this information? From very biased people who could give them very bad advice,” Dr. Pierce said.
But, getting that seat at the negotiating table takes time, and this, according to Dr. Pierce and other physicians, is where associations like the Medical Association come in and take a leadership role to make the negotiation process easier.
“Doctors are busy, literally working 60-100 hours a week in some cases, easily working more than the average person. So, it’s hard for them to take time out of their family life or professional life to get involved in organized medicine. But that’s absolutely why they should get involved. The effects of the passage of bills and restrictions on them from legislative actions or insurance company actions can be completely disruptive,” Dr. Pierce said. “That may be one of the main focuses of what the Medical Association is about, and what we do a good job of.”
Dr. Amber Clark agreed that because the mechanics of practicing medicine is moving so quickly and the rules are changing so often today, physicians cannot afford not to have a voice in that change…whether that physician agrees with the philosophy of the organization doing the advocacy work or not, it remains of the utmost importance to be involved in order to ensure the best types of changes are made for the sake of the patient and the physician.
“It’s so important to not only learn the business of medicine but to also learn how the system works. Organized medicine organizations like the AMA and the Medical Association are all doing the same thing – advocating for you and your patients. You don’t realize how important it is until you’re stuck in the middle. It’s comfortable when you operate in a bubble. It’s safe there. We will always have patients to take care of, and the only constant thing in medicine today is change. We are all intelligent beings. We don’t all have to agree on the same things. But, we’re doing a disservice to ourselves, our patients, and our colleagues to simply sit on the sidelines and be passive observers. That doesn’t mean you have to go lobby in Washington or Montgomery every day. That’s not realistic,” Dr. Amber Clark said.
Filtering out the noise.
One of the primary concerns of organized medicine is keeping members informed. Organizations act as filters or gatekeepers to allow the most important information flow to the members while keeping the noise at bay. The Medical Association’s Government Relations and Public Affairs Department works to do just that.
Dothan family physician Carlos Clark suggested not only does membership with the Medical Association give physicians a voice in the ultimate conversation about the practice of medicine and your relationship with your patient, but having a strong Government Relations team is extremely important in guiding that conversation down the best path.
“Having a strong Government Affairs department like the Association’s to stay in touch with the rest of us and help us see things coming down the pike and see things that we just wouldn’t normally see is vitally important,” Dr. Carlos Clark said. “It puts you more in tune with what’s going on. Unless you have all the free time in the world, I can’t imagine all the medical news websites you would have to search through to try to catch everything coming down the pike. Being part of organized medicine allows us to get all that information filtered so we get the most important information sent to us to act on. It’s hard enough for us to keep up with what drugs insurance companies are covering much less what rules and regulations are coming our way and when.”
Organized medicine offers more than advocacy.
For Ben Bush, who’s a medical student at the University of South Alabama College of Medicine, being a member of organized medicine and serving in leadership positions with the Medical Association and the AMA, has afforded him more opportunities in medicine than his medical school education alone could provide.
“I enjoy the relationships I’ve made. I’ve met a lot of other students and doctors from all over and created good relationships I value very much. And, there’s also the education component. I learn so much through the Medical Association and the AMA about medicine, advocacy and the practice of medicine that I can’t learn in medical school. I wanted to get involved in organized medicine primarily because of the advocacy,” Bush said.
Bush said he often gets questions from his classmates about his involvement in organized medicine, mostly concerns about why he’s participating in organizations that are often seen as not necessarily aligned with the overall beliefs of the majority of physicians treating patients today. But, he feels organized medicine is historically misunderstood and often misrepresented. In fact, he strongly encourages his colleagues who oppose medical organizations to become more involved with them.
“When my classmates ask why I’m involved in organized medicine,” Bush explained, “I tell them it’s because if I’m not a member and don’t go to those meetings to voice my opinion, then what happens? I think I’m so involved because I can voice an opinion on those policies that could negatively affect us here in Alabama. If we aren’t collectively using our voice for medicine, then the opinion we disagree with will only be that much louder, and we’ve already seen that this year in the Alabama Legislature. It’s important we defend medicine as a whole, for those in private practice to those who are employed or in academia, for every specialty…if we’re not actively moving forward to defend the practice of medicine as a whole, then we all lose.”
Dr. Pierce agreed that when involvement in organized medicine filters down to a small group, then the opinions of a small percentage of physicians are the ones expressed causing a very narrow view of the House of Medicine. As Dr. Amber Clark put it, medical students don’t graduate into any specific field of medicine, such as plastic surgery, family medicine, or gastroenterology. Being part of organized medicine means being part of medicine as a whole.
“The only way the Medical Association will ever know what the majority of physicians in the State of Alabama will need to make their practice better is if the physicians of the State of Alabama tell us,” Dr. Pierce said. “If you are not involved, you can get a small group of physicians making decisions that a majority of doctors may not believe in. That’s not good medicine, and that’s why you should be involved in organized medicine.”
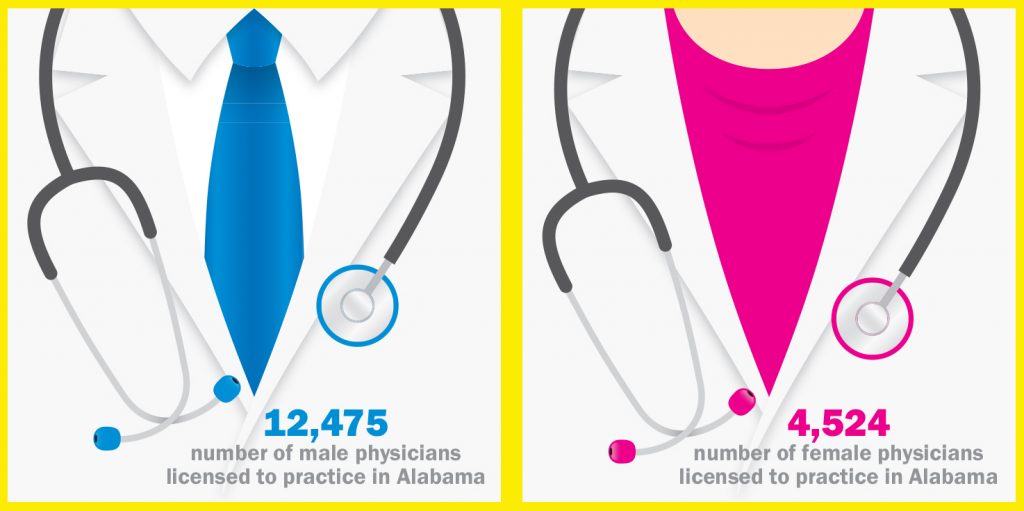
Jennifer Hayes, the Medical Association’s Director of Membership and Specialty Society Management, agreed with Dr. Pierce and equally expressed concern for the widening gap in the number of younger physicians entering practice as older physicians begin to make plans for retirement in the State of Alabama.
“The 62 percent active membership market share we have in Alabama is excellent compared to other state medical associations, the reality is our membership is aging out,” Hayes explained. “Currently, 63 percent of our membership is over the age of 50. We have to ask, how long will these physicians stay in practice?”
The Medical Association is creating avenues for residents and students to become more involved. In 2016, the House of Delegates and College of Counsellors passed a resolution to waive all dues for residents and students hoping to garner more interest in organized medicine. The Medical Association also hosts educational events and socials around the state during the year, as well as participating in medical school Match Days.
“Since the dues were waived in 2016, student membership increased 73 percent and residents 66 percent. That’s great, but we must demonstrate value and lead by example to retain these individuals who remain in Alabama. The first step for the Association has been to participate in and support their programs,” Hayes said. “Earlier this year, we created a poster symposium and Friday conference at Annual Session to allow time for networking, hear great presentations on topics related just to them, and more time with representatives from residency programs and Alabama physician recruiters. This event was so popular that we will do it again for the 2018 Annual Session with free registration and hotel scholarships. Even though the Association is making great strides to reach out to this segment of our physician base, it’s not enough. If we don’t all join together to reach out to our early career physicians, residents and students, the integrity of the Association could be in jeopardy. We have to ask ourselves one question: Are we all doing our part?”
Ultimately, it’s always about the patient.
In the end, physicians practice medicine because of their patients. Protecting the physician-patient relationship and advocating for better care for the patient is at the forefront of patient care. This puts the physician-patient relationship often at the center of most health care-related advocacy conversations in Montgomery and Washington, D.C. However, as more physicians are leaving the unified front organized medicine provides, physicians may be losing the strength to advocate for their patients and patients’ rights to the best of their abilities.
“We are losing doctor involvement,” Dr. Pierce said. “You have to have physicians involved in organized medicine or bad things could happen. These things don’t happen in a vacuum. When you’re not involved, and bad things happen, it makes it hard complain. Bad things happen because the other side is involved even more.”
As Dr. Pierce explained, a physician is the patient’s primary advocate. Even with the weight of the Medical Association behind that physician, it takes the collective of all physicians from all specialties to make a difference.
“The Medical Association does a great job of protecting our patients. But, physicians are patient advocates, too. It’s not all about me, as a person or as a physician. It’s about my patient. We have to get one thing clear – and that’s understanding the most important thing here is our patients. The focus of what you are doing as a physician is healing, and healing a patient who trusts you, who has come to you because they have a relationship with you. Ultimately, it’s always about the patient, and we cannot ever forget that.”
Article by Lori M. Quiller, APR
Director of Communications and Social Media



 Dr. Bradley Wills, who originally received first place at the Medical Association’s Second Annual Poster Symposium in April for his poster entitled Outcomes with Overlapping Surgery at a Large Academic Medical Center, presented his research poster at the 2017 AMA Interim Meeting in Honolulu in November and won the Resident-Fellow Section Division for Clinical Medicine.
Dr. Bradley Wills, who originally received first place at the Medical Association’s Second Annual Poster Symposium in April for his poster entitled Outcomes with Overlapping Surgery at a Large Academic Medical Center, presented his research poster at the 2017 AMA Interim Meeting in Honolulu in November and won the Resident-Fellow Section Division for Clinical Medicine.
 Centreville physician John Waits was the only Alabama physician to be recognized by the National Organization of State Offices of Rural Health’s 2017 Community Stars Program. Dr. Waits was one of 31 honorees during the 2017 National Rural Health Day working tirelessly to improve, protect and advance health and wellness in our rural communities.
Centreville physician John Waits was the only Alabama physician to be recognized by the National Organization of State Offices of Rural Health’s 2017 Community Stars Program. Dr. Waits was one of 31 honorees during the 2017 National Rural Health Day working tirelessly to improve, protect and advance health and wellness in our rural communities.
 While encouraged to attend many of the general sessions, such as the Ellann McCrory, M.D. Leadership Lecture with Auburn University Basketball Coach Bruce Pearl and the Jerome Cochran, M.D., Lecture with James B. McClintock, Ph.D., concurrent sessions were set aside to engage these young physicians just starting their medical practice. Medical Association Partner Regions Bank offered two sessions, Banking Basics for Residents and Students and Maximizing Your Personal Wealth, while Sirote & Permutt, P.C., discussed Contract Negotiations. Zalak Patel, M.D., with the UAB School of Medicine, Montgomery Regional Medical Campus, offered a hands-on Basic Airway Management Skill Session.
While encouraged to attend many of the general sessions, such as the Ellann McCrory, M.D. Leadership Lecture with Auburn University Basketball Coach Bruce Pearl and the Jerome Cochran, M.D., Lecture with James B. McClintock, Ph.D., concurrent sessions were set aside to engage these young physicians just starting their medical practice. Medical Association Partner Regions Bank offered two sessions, Banking Basics for Residents and Students and Maximizing Your Personal Wealth, while Sirote & Permutt, P.C., discussed Contract Negotiations. Zalak Patel, M.D., with the UAB School of Medicine, Montgomery Regional Medical Campus, offered a hands-on Basic Airway Management Skill Session. Community Hospital, Inc., (General Surgery, Radiology and Transitional Year)
Community Hospital, Inc., (General Surgery, Radiology and Transitional Year)