Tag: claim
-

Fewer Physicians Could Be Audited under a New CMS Program
Fewer physicians will undergo audits under a new Medicare claims review process, according to a Centers for Medicare & Medicaid Services announcement. CMS will roll out a new approach to claims review nationwide targeting fewer providers and requiring review of fewer claims. The new policy, to take effect later this year, makes it less likely…
-
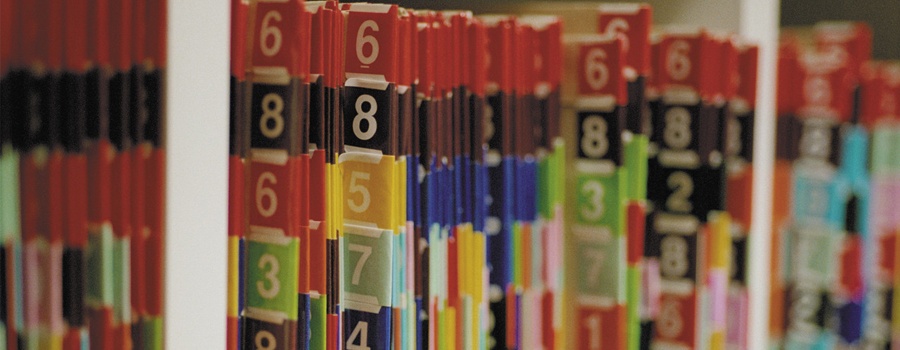
A Refresher in the Medicare Claims Appeals Process…
With the increased audit activity we are seeing among the alphabet soup of Medicare contractors – RACs, ZPICs, SMRCs, CERTs, etc. – now appears to be a good time for a refresher on the Medicare claims appeals process. Due to this increased audit activity, more and more claims are being denied, both under pre-payment review…
-

Close Patient Care/Diagnosis Gaps with New Informational Claim Process
Blue Cross and Blue Shield of Alabama now offers a new informational claim process in which you have the option to submit an informational claim through ProviderAccesseClaims to report previously closed patient care/diagnosis gaps. The informational claim is for reporting purposes only. Effective March 6, 2017, the option to dispute an item on a patient’s…
