Tag: drug
-

Drug Overdoses in Young People on the Rise
PISCATAWAY, NJ – In American adolescents and young adults, death rates from drug poisoning, particularly from opioids, have sharply increased over the last 10 years, according to new research in the Journal of Studies on Alcohol and Drugs. In 2006, the death rate from drug poisoning from any type of legal or illicit drug was 8.1…
-

President Trump Signs Right-to-Try Act
On Wednesday, May 30, 2018, Pres. Donald Trump signed the Right-to-Try Act, which allows terminally ill patients the ability to try drugs in preliminary testing but not-yet-approved by the Food and Drug Administration. The aim is to make it easier for those patients suffering from fatal illness who have exhausted all other resources to access…
-
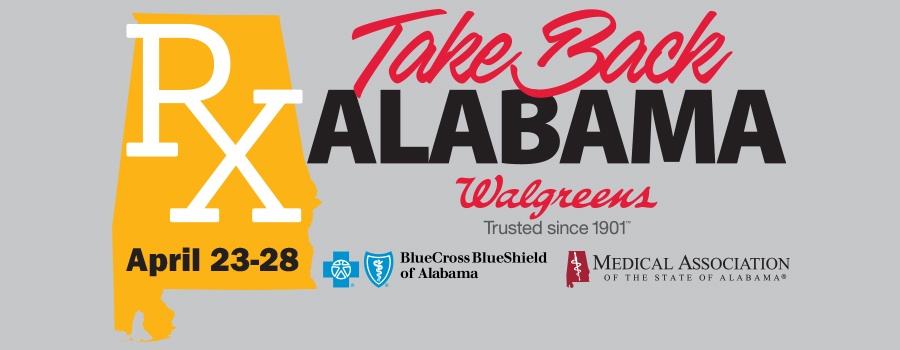
Successful Take Back Alabama Week Ends with Opioid Summit
REVISED APRIL 27, 2018 ─ The Medical Association’s Take Back Alabama Week kicked off this week with a press conference at Walgreens in Birmingham on Monday, April 23. Representatives from AmerisourceBergen, Blue Cross and Blue Shield of Alabama, Pfizer, Prime Therapeutics and Walgreens joined Attorney General Steve Marshall and Birmingham physician Gregory Ayers to announce…
-

Alabama SB39: Another Shot in the Opioid Battle
On March 28, 2018, Alabama Senate Bill 39 was sent to Governor Ivey’s desk for signature. SB39 introduces stiffer penalties related to fentanyl possession and distribution. It amounts to a local effort forming part of a nationwide, multi-pronged response to the opioid epidemic that has plagued the country in recent years. While this bill is…
-

Just What the Doctor Ordered: An Alabama Perspective on the Opioid Epidemic
Sometimes, Alabama is No. 1. In 2012, Alabama was the highest per capita painkiller prescribing state, with an average of 143 prescriptions written per 100 people — almost three times the rate of the lowest prescribing state.1 Alabama has been home to other No. 1s, too. In 2012, Dr. Shelinder Aggarwal, a former Huntsville-area pain…
-

FDA Classifies Kratom as Opioid
The U.S. Food and Drug Administration has officially classified the plant kratom, originally seen as an opioid alternative, as an opioid itself, stating that compounds in kratom act like prescription-strength opioids. Found in Malaysia, the leaves of the kratom plant are traditionally crushed and made into a tea to treat pain as well as heroin…
-

Medical Association’s 2018 State and Federal Agendas
The Medical Association Board of Censors has met and approved the Association’s 2018 State and Federal Agendas. These agendas were developed with guidance from the House of Delegates and input from individual physicians. As the Alabama Legislature and U.S. Congress begin their work for 2018, additional items affecting physicians, medical practices and patients may be…
-

CDC Reports Rising Rates of Drug Overdose Deaths in Rural Areas
Rates of drug overdose deaths are rising in nonmetropolitan (rural) areas, surpassing rates in metropolitan (urban) areas, according to a new report in the Morbidity and Mortality Weekly Report (MMWR) released this week by the Centers for Disease Control and Prevention (CDC). Drug overdoses are the leading cause of injury death in the United States,…
-

Congress Squares Off Over Drug Pricing and a Controversial Drug Discount Program
House Democrats are calling foul on Republican assertions that cuts to a little-known discount drug program will eventually reduce skyrocketing drug prices. At a hearing Tuesday, Rep. Diana DeGette (D-Colo.) said high drug prices should be investigated separately from the focus on oversight of the drug discount program, known as 340B. “I think we need…
-

Public Restrooms Become Ground Zero in the Opioid Epidemic
A man named Eddie threaded through the midafternoon crowd in Cambridge, Mass. He was headed for a sandwich shop, the first stop on a tour of public bathrooms. “I know all the bathrooms that I can and can’t get high in,” said Eddie, 39, pausing in front of the shop’s plate-glass windows, through which we…