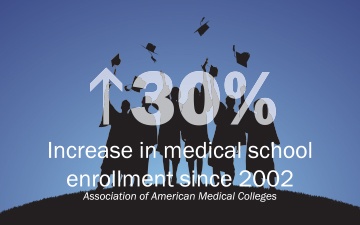
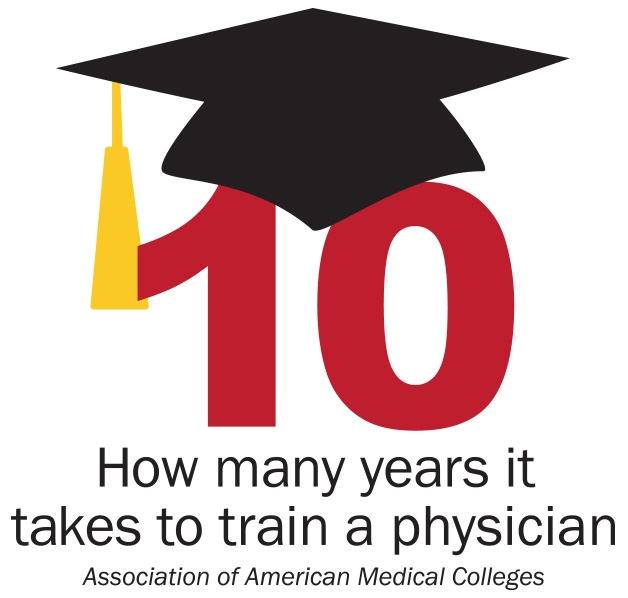
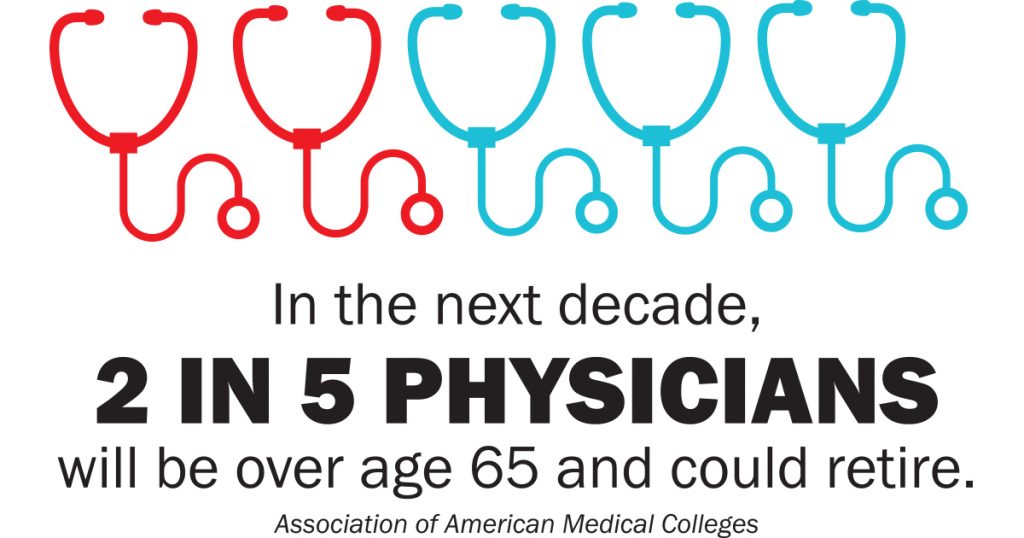
 It takes up to 10 years to train a physician. That decade of training is just one contributing factor for the reason the United States is facing a serious shortage of physicians. Other factors include the growth and aging of the population and the impending retirements of older physicians. While medical schools have increased enrollment by nearly 30 percent since 2002, the 1997 cap on Medicare support for graduate medical education has stymied increases in the number of residency training positions, which are necessary to address the projected shortage of physicians.
It takes up to 10 years to train a physician. That decade of training is just one contributing factor for the reason the United States is facing a serious shortage of physicians. Other factors include the growth and aging of the population and the impending retirements of older physicians. While medical schools have increased enrollment by nearly 30 percent since 2002, the 1997 cap on Medicare support for graduate medical education has stymied increases in the number of residency training positions, which are necessary to address the projected shortage of physicians.
A 2019 study conducted for the Association of American Medical Colleges by IHS Markit predicts the United States will face a shortage of between 46,900 and 121,900 physicians by 2032. There will be shortages in both primary and specialty care, and specialty shortages will be particularly large.
Unfortunately, the State of Alabama is already experiencing a physician shortage, most notably in rural areas, and to make matters worse Alabama ranks in the last five of 50 states in health status categories.
Even with Alabama’s medical schools working to educate and nurture a future crop of physicians, there’s no guarantee these medical school graduates will remain here through their residencies or return to Alabama to practice medicine should they complete residencies outside of the state.
In 2018, the Pickens County Medical Society introduced a resolution at the Medical Association’s Annual Business Session to create a planning task force to develop and restore adequate health care manpower with a specific focus on Alabama’s rural areas. The resolution stands as a reminder that while primary care medicine is effective in raising health status, supporting hospitals and improving the economic status of disadvantaged communities, the state’s aging population is also causing an escalation in need for primary care physicians.
“The task force has brought together physicians from across the state with various practice situations to work with the many entities that comprise our health care system,” said Beverly Jordan, M.D., a family and sports medicine physician from Enterprise, Ala., who chairs the task force. “Both long
and short-term goals are being developed, and we look forward to expanding our work to non-physician groups that play an essential role in the development and sustainability of physicians in rural Alabama. A variety of barriers to physician practice in rural Alabama have already been identified, as well as several amazing programs that address those barriers and ideas for innovative solutions.”
Members of the task force met in person for the first time in August 2018 and discussed a number of issues but focused on the importance of fully funding the Board of Medical Scholarship Awards, scope of practice, physician pipeline programs, education and the possibility of GME expansion, recruitment and retention of physicians through meaningful tax credits and rural community support, and start-up business models.
Medicaid Commissioner Stephanie Azar and Dave White from the Governor’s Office joined the meeting to hear the concerns of the task force and take their report back to Gov. Kay Ivey.
“Because this was the first face-to-face meeting of the task force, we had a lot of ground to cover,” said Executive Director Mark Jackson. “Naturally there are a lot of concerns about health care shortages in rural areas, but our goal is a long-term solution. The members of the task force realize this isn’t an easy fix, which is why they were willing to express their concerns openly and honestly to the Governor’s staff.”
This year during the Annual Business Meeting the task force offered a report of its first year’s work including a number of initiatives to improve the rural primary care workforce, new and proposed initiatives, and future recommendations.
What Are We Doing NOW to Improve the Rural Alabama Primary Care Physician Network?
There are already a number of initiatives in place designed to improve the rural physician workforce in Alabama. These have proven successful in the past, yet given the growth trends in population and fewer physicians are choosing to locate to rural settings, these initiatives will not be enough to sustain adequate access to care for our residents living in rural areas:
Alabama Board of Medical Scholarship Awards Amended in 1994, this legislative program was funded at about $1.4 million in 2018. Funding currently allows about nine recipients a year (full cost of medical school attendance), with a significant waiting list. As a result, 96 percent of recipients practice in Alabama; 98 percent in primary care (78 percent family medicine); 90 percent in rural Alabama; 73 percent continue in their original communities after completing the scholarship obligation.
Physician Tax Credit Act The State of Alabama allows a state income tax credit of $5,000 for up to five years for a physician or dentist in rural practice. Legislation is currently being considered to enhance the tax credit. The Medical Association staff will report on any changes to this legislation as the Regular Session of the Alabama Legislature continues.
Rural Medical Scholar Program (RMSP) Since 1996 this program has enjoyed statewide and national acclaim as a successful model for rural college students through medical school. On average, 11 students are admitted to this highly selective five-year medical education program of The University of Alabama and the University of Alabama School of Medicine. The Rural Medical Scholars Program includes a year of study, after students receive their undergraduate degree, that leads to a master’s degree in Rural Community Health and early admission to the School of Medicine. Undergraduates may qualify after their junior year if they have met most of the requirements for their undergraduate major. In the year prior to entry into medical school, students take courses related to rural health and the practice of primary care in rural areas, and participate in special seminars, field trips and community service programs. Since its founding in 1996, more than 200 students have participated in the program, and of the graduates, 81.8 percent practice in Alabama while 62 percent practice in rural Alabama.
Rural Medical Program (RMP) The Rural Medical Program began in 2005 and is modeled after the RMSP. This five-year medical school curriculum’s sole purpose is the training of physicians to serve in the areas of greatest necessity. RMP is a jointly sponsored program by the Auburn University College of Sciences and Mathematics and UAB School of Medicine Huntsville Regional Campus. The RMP curriculum promotes family medicine by providing for students to attend the annual meetings of the Alabama Academy of Family Practice and the National Student American Academy of Family Practice. Students also participate in the Medical Association’s Governmental Affairs Conference in Washington, D.C. The program has 79 percent of graduates that are family physicians, 90 percent are in primary care practice, and 74 percent are rural.
Early Medical and Other Health Professions Pipeline Programs Rural Health Scholars, Rural Minority Scholars and others have sought to provide high school and community college student recruitment and guidance. Tuscaloosa’s Rural Minority Health Scholars has had 200 members and 15 have gone to medical school. Of the 650 Rural Health Scholars from 1993-2018, 56 have gone to medical school. These programs are aimed at all health care occupations and serve to raise awareness of medical opportunities for hundreds.
Huntsville Rural Premedical Internship (HRPI) Since 2004, by bringing college students with rural backgrounds to the UAB Huntsville medical campus for a summer experience including clinic shadowing, didactic sessions, field trips, and medical skill workshops. With 74 percent of available graduates being accepted to medical school (125/169); 67 percent of participants having completed medical school and residency are in primary care; 67 percent are in Alabama with 46 percent rural. Of those in HRPI and a rural track such as RMP or RMSP, 75 percent are rural Alabama family physicians.
Alabama Area Health Education Centers (AHEC) Started in 2012, five centers across Alabama focus on improving access and workforce in rural and underserved communities. AHEC engages in student recruitment and support and physician education and retention activities, partnering with medical and other health professions schools to link students to positive clinical rotations in underserved areas. Revised HRSA funding directions have decreased support for this level of activity by AHEC, through its centers continue to address these goals through other support. Improved networking, information and digital resources may provide leverage for these important but challenging activities.
Medical School Admissions Committees Important factors include student recruitment, school policies and priorities for recruiting rural and underserved students, and committee membership (particularly rural and family physicians). The Medical Association can provide opportunities for expanded dialogue with our medical schools about how to increase the number of rural medical students, utilizing successful models from our own state and others. Using these current programs and initiatives as benchmarks, the task force began to work outward searching for changes and new models to reinforce what was already working and expand opportunities for new physicians in rural areas.
“The most important fact about this rural task force is that the Medical Association is stepping up to the plate to address the wide range of problems and challenges facing rural health in our state. That’s a highly responsible and even courageous act. The last time our Association did this was more than 20 years ago, and the outcome was the modern version of the Medical Scholarship Act and our current collaborative model for advanced practice providers such as nurse practitioners and physician assistants,” said Bill Curry, M.D., Dean of Rural Programs for University of Alabama Birmingham School of Medicine and one of the chairs of the Manpower Shortage Task Force. “This time, Dr. Jordan and the Board have taken a comprehensive and long term approach. We’re looking at everything from the physician workforce pipeline – reaching from rural schools through college, medical school, residency, and practice recruitment and retention – to the plight of rural hospitals to the responsibilities of our medical schools and state agencies to partner with communities and professional societies across all that’s involved in rural health. It’s a very full plate, and it’s important to identify initiatives with impact and to set priorities.”
The Next Step
Fact: During the last five years nationwide, applications to and enrollment in medical schools have increased.
Fact: While there is a projected shortage of primary care physicians, there is also a projected shortage of specialists.
Fact: Fixing the physician shortage requires a multipronged approach including innovations in team-based care and better use of technology to make care more effective and efficient.
Facing the facts of a physician shortage is the first part of the battle. The members of the Manpower Shortage Task Force had the opportunity to define new initiatives to begin to create a path to move the state forward and away from a deficit of physicians in rural areas.
Practice Incubator Models Multiple partnerships involving existing or new practices, health systems and local governments, with or without initial support through the Alabama Board of Medical Scholarship Awards, the National Health Service Corps, or other scholarship programs. The incubator process involves recruitment of mentee doctors (frequently just out of training) to rural practices established by mentors. The mentee then learns private practice and is subsequently enabled to move to another rural location by the mentor or the mentee may simply buy into the existing practice if sufficient growth has occurred. The benefit to the mentor is a return on investment of satellite practices or income realized above the salary of the mentee.
Improved Workforce Database Traditional sources of information about the Alabama physician workforce include the Alabama Board of Medical Examiners, the American Medical Association physician database, the American Academy of Family Physicians, the National Rural Health Association, County Health Rankings, the Center for Medicare and Medicaid Services, and information from the Alabama Department of Industrial Relations. Recently the UASOM Huntsville Office for Family Health, Education and Research (OFHER) has combined, analyzed and displayed data from various sources into more usable and interactive formats, and the Alabama Rural Health Association has collaborated in this effort also.
Improve and Standardize the Designation of Primary Care Shortage Areas for Alabama HRSA has established a work directive for all state Offices of Primary Care (PCOs) to establish a state network of rational service areas for identifying local and/or regional shortages and developing rational and reasonable solutions to eliminate identified shortages. The Alabama medical community must be a major player in the development of Alabama’s Rational Service Areas (RSAs). There is a major concern if the Medical Association and the medical community are not involved in the formation of state RSAs, then private practice primary care providers and physician mental health providers and rural hospitals will be left out.
Scholarships Graduate medical education programs in primary care need more scholarships. Some scholarships expect recipients to enter primary care while others require rural service. Currently, the BMSA is the most successful program in the state, and possibly the nation, for providing physicians to rural areas. The scholarship is repaid by rural service of four to six years depending upon the size of the underserved town.
Changes in Undergraduate Medical Education Students most likely to enter rural practice are those from rural areas. Selecting students from rural Alabama, expanding rural premedical programs, and expanding the rural tracks will provide a larger pool of applicants to the state’s family medicine residencies. Other options include allowing early admission as college juniors providing they achieve predetermined academic and MCAT standards; and placing third-year students with primary care physicians, which serve to increase student familiarity and comfort with the practice.
Changes in Graduate Medical Education Data shows the physician most likely to practice in Alabama is one who is from Alabama and who attends medical school and residency here. Also, the person who is from a rural area in the state is the most likely to return to a rural area. The most important mission is to fill the current family medicine slots with the Alabamians most likely to enter rural practice. New residency programs are also an option. These programs are beginning to pop up across the state from Madison County to Baldwin County in a variety of specialties.
Transition from Residency to Practice The final chapter of the process is moving from a residency to a medical practice. The expansion of the BMSA is the surest and fastest method of attracting physicians (which has solid, objective data proving its worth). Out-of-state physicians may be attracted to rural Alabama because of the advantages in cost of living and professional satisfaction. Physicians may move from states ranked as the worst in which to practice medicine (IL, CA, MD, OR, MA, DC, NY, RI, NM and NJ) to Alabama, which was ranked the third best in the U.S. behind NC and TX. (Medscape Physician Survey, 2016).
Targeting the Black Belt Communities According to the Black Belt Solutions/Community Engagement Subcommittee’s Co-chair John Wheat, M.D., engagement and partnerships among communities and resource agencies for this area will be the lynchpin for its success.
“This population and region desire doctors and other health professionals who understand their life, identify with them, and want to live and practice among them,” Dr. Wheat explained. “It is apparent such physicians are far more likely to be from the Black Belt than elsewhere, their course through medical education must be supported in many ways, that practice facilities must be on par with urban counterparts, that social and professional contexts must be prepared for them, and patients must be able to afford to come to them. Our first and continuing task is to engage the knowledge, trust and commitment of multiple groups with varying perspectives and influences for making changes required to succeed in these efforts.”
Dr. Wheat and co-chair Brittney Anderson, M.D., are originally from Alabama’s Black Belt and have begun reaching into the community to contact local ministers, county commissioners, physicians who grew up in the region, and other community activists with strong commitments to the region for opinions and ideas about how to better serve the area.
“We have been well received and encouraged to continue toward setting up a planning structure that will be inclusive and unify multiple groups and agencies. We look forward to having a planning group that will receive enthusiastic invitations from various Black Belt communities asking us to partner with them in producing and maintaining the health care professionals in their community,” Dr. Wheat said.
The Long Road Ahead…
The Medical Association and the members of the Manpower Shortage Task Force realize there is a long road ahead to finding the best solutions to Alabama’s physician shortage in our rural areas, but we are working toward solutions…and there will be many solutions and many partners to take part in the process.
“We recognized that without a viable rural health system – which has to include either a hospital or a freestanding facility with after-hours and emergency coverage – it’s difficult or impossible to have effective primary care and other services in a rural community,” Dr. Curry said. “The Association’s reaching out to the Alabama Hospital Association and other partners is a huge step, and I hope the regulatory or other changes needed will happen soon.”
Dr. Jordan agreed, adding that help from established physicians is always welcome.
“Our work has just begun, and we look forward to continued efforts to both develop and sustain excellent health care communities in rural Alabama,” Dr. Jordan said. “As we expand our workgroups to include educational, business, political and religious leaders in our state, we welcome the involvement of our physician members. Please don’t hesitate to contact us if you are willing to help – we need you!”
If you would like to be involved with the task force, have questions, or would like to contribute an idea, please email Association Executive Director Mark Jackson.