You can still avoid the MIPS 4 percent penalty by participating this year!
In 2017 the TEST portion of MIPS allows a provider to submit one Quality measure (previously known as PQRS) for less than a 90 day period to potentially avoid a 4 percent MIPS penalty (to be incurred in 2019) on Medicare Part B claims. One example of this is G8427 – Current Medications Documented. Every office typically documents a patient’s Current Medications. If you submit this code on your claims, even if only for a short period of time, you will be participating in the test portion of MIPS and may avoid a 4 percent penalty on Medicare Part B in 2019.
Remember, you will need to do this for every TIN/NPI combination in your practice.
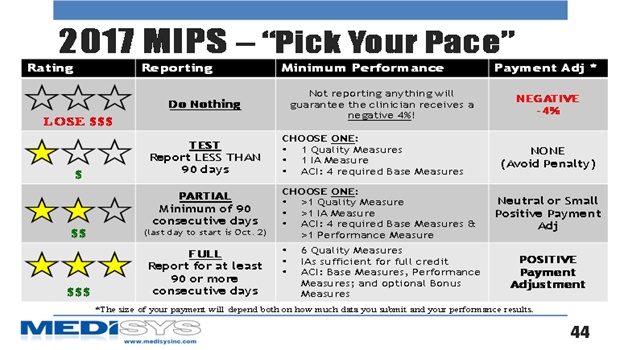
The graph below shows a broad overview of the current MIPS attestation guidelines. Each line gives a brief summary of the four different attestation paths an office can choose from for 2017. Based on your 2017 participation, the above information references the row with one star and explains the simple criteria required this year to easily avoid a 4 percent penalty which incurred in 2019.
Need help understanding these new MIPS requirements? Contact MediSYS today at 1 (334) 277-6201 or email questions to sales@medisysinc.com. Our staff has been assisting practices with various CMS incentive programs since their inception. We combine years of experience with ongoing support and detailed expertise for our clients at no additional support charges.
For information on MediSYS electronic health records and practice management solutions as well as outsourcing CCM services, please contact MediSYS at sales@medisysinc.com and visit the website at www.medisysinc.com. MediSYS is an official partner with the Medical Association.
