Tag: appeal
-
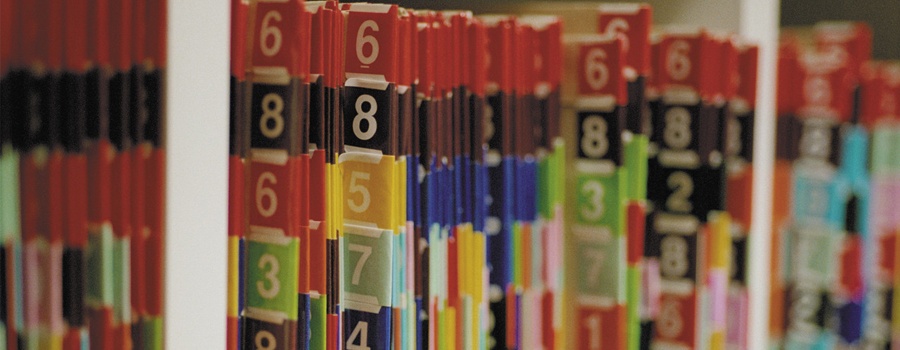
A Refresher in the Medicare Claims Appeals Process…
With the increased audit activity we are seeing among the alphabet soup of Medicare contractors – RACs, ZPICs, SMRCs, CERTs, etc. – now appears to be a good time for a refresher on the Medicare claims appeals process. Due to this increased audit activity, more and more claims are being denied, both under pre-payment review…
-

Florida’s Physician “Gun Gag” Overturned on Appeal
The full panel of the U.S. Court of Appeals for the 11th Circuit struck down the Florida law restricting physicians from speaking to patients and families about the risks of guns in the home. The case, Wollschlaeger v. Scott, was filed on June 6, 2011, challenged the Florida law, which could censor, fine and revoke…